Your gut might not be the first place you look to find the root of your autoimmune disease, but as your body's second brain, your gut microbiome is closely connected to your immune system.
In fact, your gut microbiome influences and interacts with multiple aspects of your health, including your mood and metabolism. That’s why it’s so important to maintain a balanced microbiome that has diverse colonies of beneficial disease-fighting bacteria.
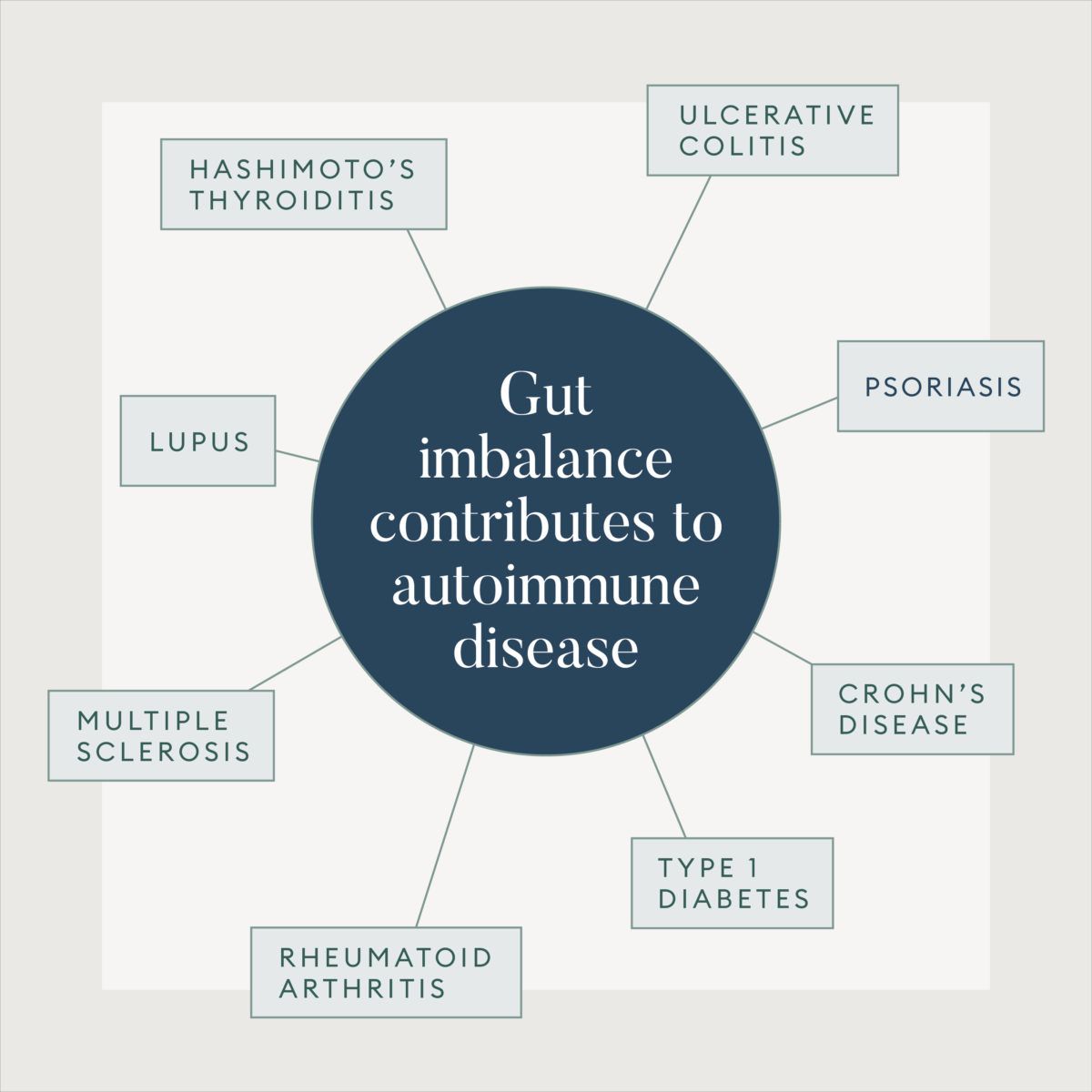
“While bacteria colonize the whole body, such as the oral cavity, placenta, vagina, and skin, the majority of bacteria resides within the gastrointestinal tract,” explains Gabriella Safdieh, MD, a board-certified pediatrician and rheumatologist formerly at Parsley Health New York. “Unfortunately, dysbiosis—or an imbalance between good and bad bacteria in your gut—has been associated with numerous diseases, including autoimmune diseases like Crohn’s and ulcerative colitis, psoriasis, lupus, and multiple sclerosis."
What is autoimmune disease?
An autoimmune disease is a condition in which your immune system mistakenly attacks your body. Normally, when a virus or bacterial infection starts to invade the body, your immune response is to produce antibodies that work against these harmful microorganisms. But with autoimmune disease, the body creates autoantibodies that end up attacking the cells they're supposed to protect. As autoimmune disease becomse more common, the U.S. Department of Health and Human Services reports that more than 23.5 million Americans live with an autoimmune disease.
Autoimmune diseases are more common in women, especially those of childbearing age, than in men, and certain ethnic groups are more susceptible than others. For example, African American, Hispanic, Asian, and Native American women are two to three times more likely to develop lupus than Caucasian women, according to the American Autoimmune Related Diseases Association. Some of the most common autoimmune diseases in women are alopecia areata, celiac disease, type 1 diabetes, and Graves’ disease. Although it’s largely unclear why autoimmune diseases affect more women than men, some studies show that testosterone in men offers some protection. A May 2018 study in Nature Communications suggests that testosterone suppresses the protein BAFF, which makes B cells—lymphocytes that release harmful antibodies—linked to autoimmune diseases like lupus.
Scientists aren’t really sure what causes autoimmune disease, but researchers believe that there are a number of contributing factors, including genetics and environmental exposures. Having a family history of autoimmune diseases, for example, can increase your risk of developing the disease. According to the U.S. National Library of Medicine, another theory is that microorganisms or drugs may trigger changes that confuse the immune system. Exposures to certain chemicals and viral and bacterial infections are also linked with autoimmune diseases.
How your gut microbiome is connected to autoimmunity
There is a growing body of research that has linked autoimmune issues to the health of the gut microbiome. Because 80 percent of your immune system is within the gut lining, any imbalances you have in your microbiome can contribute to the development of an autoimmune disease, Dr. Safdieh says. A January 2017 review in BMC Immunology demonstrates the effects of dysbiosis and its relationships with autoimmune disorders, like inflammatory bowel disease, type 1 diabetes, and rheumatoid arthritis. Pro-inflammatory microbes in the gut can result in immunosuppression and also lead to a disease beyond the gut, such as the heart, liver and nervous system.
Environmental factors, such as the overuse of antibiotics, can also affect the bacteria in the gut and increase the risk of autoimmune disease, suggests a review in Gut Microbes. “Overuse of antibiotics and pharmaceuticals has caused a drastic reduction in the diversity of our collective microbiome,” Dr. Safdieh says. Having a leaky gut, in which there is inflammation and weakening of the gut barrier, is also associated with exposure to certain chemicals and drugs connected to autoimmunity.
Studies have even shown that pre- and post-natal factors can shape the development of your microbiome, which impacts your risks of developing an autoimmune disease. “Our microbiomes start forming as early as birth during delivery,” Dr. Safdieh says. “Babies are exposed to maternal flora as they come through the vaginal canal. Infant feeding methods and breastfeeding earlier in life also play a role in the infant’s microbiome development,” she says. For example, Dr. Safdieh says that at Parsley, pregnant women and mothers who have Guillain-Barre Syndrome (GBS), a rare autoimmune disease, are treated without antibiotics to keep their guts robust, and in turn, helps keep their babies healthy.
For example, a July 2016 review article in Nature Medicine points out that one of the first major exposures to microbes in newborns is during the birthing process. During vaginal births, a mother’s vaginal microbiota is transferred to the child, enriching them with good bacteria like Lactobacillus spp. However, babies born via C-section don’t receive this benefit and are colonized by common skin and environmental microbes, like Staphylococcus and Streptococcus. This puts infants born via C-section at higher risk for developing dysbiosis. Infants born via C-section have also been shown to have greater rates of asthma, allergies, obesity, and autoimmune disorders than those born vaginally, a February 2016 study in The Journal of Allergy and Clinical Immunology shows.
Breastfeeding and maternal health play a role in risk of autoimmune disease too. A May 2018 review article in Frontiers in Medicine points out that the mother’s health circumstances for infants delivered via C-section could have an impact on their gut health and autoimmunity risks. Mothers who are delivering via C-sections are sometimes administered antibiotics, which can affect an infant’s microbiome. C-section deliveries are also associated with poor breastfeeding behavior. Breast milk contains a variety of important nutrients that influence an infant’s gut microbiome. “Many babies, unfortunately, aren’t fed right away because of NICU stays and surgeries,” Dr. Safdieh says. In addition, maternal obesity is a risk factor for C-section delivery, so there’s a chance that it can alter the infant’s gut microbiome pre- and post-natal.
Lifestyle factors that affect the gut and autoimmunity
While you may not be able to control your birth mode or potential genetic factors that influence gut health and autoimmunity, your lifestyle can have a profound effect on your gut and contribute to autoimmunity. “Stress and anxiety, as well as what we eat, can affect the composition of the gut bacteria. Sleep loss can also lead to changes in the microbiome and promote gut inflammation,” Dr. Safdieh says. “Stress has an impact on the microbes within our guts, and the balance of microbes has an effect on our moods. That’s because 75 percent of our neurotransmitters are made within the gut."
This includes serotonin, which plays a role in happiness, Dr. Safdieh says, so it has a big impact on mental health. A large cohort June 2018 study in JAMA showed that patients with stress-related disorders, such as post-traumatic stress disorder (PTSD) and acute stress disorder, have an increased risk of autoimmune disease. It’s believed that trauma and significant life stressors can disrupt the nervous system, which can dysregulate immune function and manifest as an autoimmune disease. The study also found that among patients with PTSD, those who persistently used SSRIs (selective serotonin reuptake inhibitors) during the first year after diagnosis was associated with a risk of autoimmune disease. This circles back to the idea that certain drugs and medications may trigger autoimmunity.
Could your autoimmune disease be caused by a gut issue?
At Parsley Health, doctors like Dr. Safdieh might evaluate a member's stool samples to get a better glimpse into their microbiome if they suspect gut health is at the root of an autoimmune condition. “We look at the diversity of bacteria, overgrowth of pathogenic, or bad, bacteria, overgrowth of yeast, undergrowth of good bacteria, levels of inflammation and levels of yeast overgrowth,” Dr. Safdieh says. Doctors will use advanced tests that are more comprehensive than the stool sample routinely done at offices to simply look for blood or infection, she explains. These gut microbiome tests give doctors an insight into whether you have inflammation in the digestive tract, which can indicate autoimmune issues.
If you’re dealing with gut problems or an autoimmune disease, working with a trained physician at Parsley Health can help you restore balance in your microbiome and prevent and manage autoimmune flare-ups when they occur. Here, Dr. Safdieh shares some ways she would treat autoimmune issues that have a root cause in the gut.
Autoimmune disease treatment for issues that stem from the gut
Follow an anti-inflammatory diet
Dr. Safdieh says that the first step in creating and maintaining a healthy gut microbiome is to limit inflammatory foods, such as gluten, dairy, refined sugar, and processed foods. You want to fill up on foods that will nourish your gut, like vegetables, fruits, and fermented foods. “Some individuals with autoimmune disease choose to follow the Autoimmune Paleo Diet (AIP), which is thought to reduce flare-ups from autoimmune disease,” Dr. Safdieh says. This autoimmune disease diet involves following a food elimination phase for at least 30 days and a reintroduction phase of slowly reintroducing foods that don’t trigger symptoms. Grains, dairy, processed vegetable oils, processed foods and nightshade produce are among the eliminated foods. But it also emphasizes eating plenty of quality protein, healthy fats, vegetables, and fermented foods to boost gut health. The health coaches at Parsley Health are trained to work with people with an autoimmune disease who want to follow the AIP diet.
Take a high-quality probiotic
It’s important to re-populate the gut microbiome with good strains of bacteria if you have autoimmune issues, Dr. Safdieh says. She’ll work with patients to determine the best strains and dosage of probiotics for them based on their needs. But some strains she’ll recommend are lactic acid bacilli, such as Lactobacillus and Bifidobacterium, a nonpathogenic strain of Escherichia coli (E. coli Nissle), Clostridium butyricum, Streptococcus salivarius, and Saccharomyces boulardii.
Consider fecal transplants
Some clinics perform fecal transplants to reset the microbiome in people with autoimmune disease. “This is specifically becoming more frequent in people with Crohn’s disease and ulcerative colitis,” Dr. Safdieh says. Talk to your doctor to see if you can benefit from fecal transplants.
Manage stress and anxiety
It goes without saying but keeping your stress levels down and finding time to unwind will help your gut in the long-term and help prevent flare-ups. Whether it’s exercise, meditating, journaling, doing yoga, or taking a relaxing bath, be sure to carve out space in your schedule to de-stress.

