Hashimoto’s disease most commonly leads to an underactive thyroid, but symptoms don’t always stay consistent. Many people experience periods when symptoms suddenly worsen, often referred to as Hashimoto’s flare-ups. During a flare, fatigue, brain fog, mood changes, and other symptoms can intensify, sometimes seemingly without warning.
Hashimoto’s is an autoimmune condition in which the immune system produces antibodies that attack the thyroid, a small butterfly-shaped gland at the base of the neck that plays a key role in metabolism, energy, and hormone regulation. Over time, this immune response can affect how well the thyroid functions, contributing to cycles of relative stability followed by symptom flare-ups.
So what does a Hashimoto’s flare-up actually feel like, and how long do flare-ups last? While experiences vary from person to person, there are common patterns, symptoms, and triggers that can help explain what’s happening in the body.
In this article, we’ll walk through the most common Hashimoto’s flare symptoms, what may trigger a flare, how long flare-ups typically last, and practical ways to support your body through them using a root-cause, whole-body approach.
What is a Hashimoto’s flare-up?
Before we dive into Hashimoto's attack, let's take a step back: What are autoimmune flare-ups in general? A flare-up occurs when symptoms suddenly and swiftly return, and while they can look like the symptoms you normally experience, flare-ups tend to be more severe.
Just as you’ve been coasting along and feeling pretty great, you’re hit again with familiar symptoms. Maybe you haven’t pooped in days. You’re suddenly cold and wearing your “summer sweaters.” You’re mopey as heck, and no number of naps can relieve the unrelenting fatigue.
Flares happen because of additional stress on your body, which taxes an immune system that is already hyper-vigilant, sending it into a tailspin. “When flares happen, there is a greater antibody response going on at that time, which leads to more destruction of the thyroid gland,” says Neeti Sharma, MD, a board-certified internal medicine physician at Parsley Health.
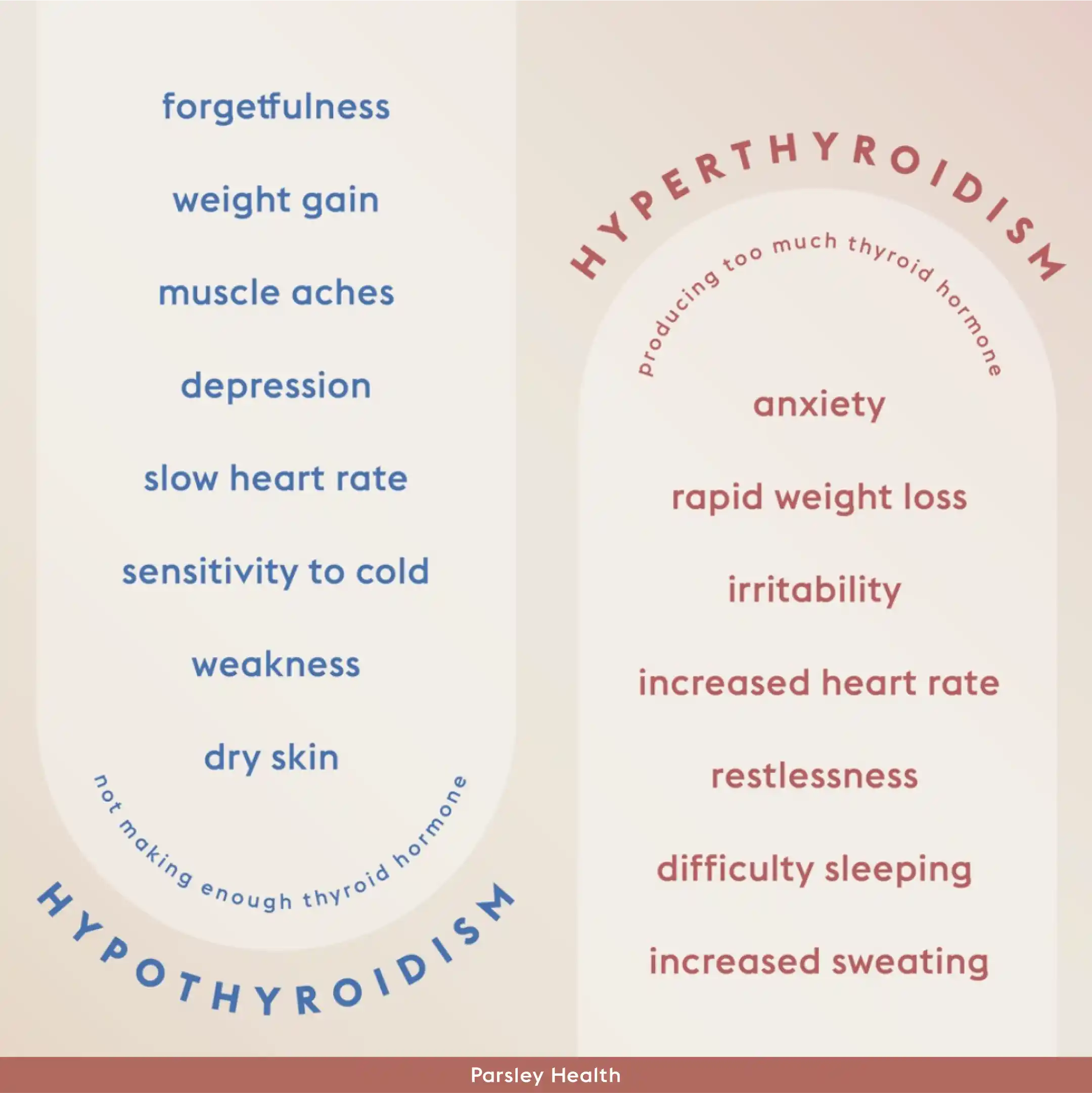
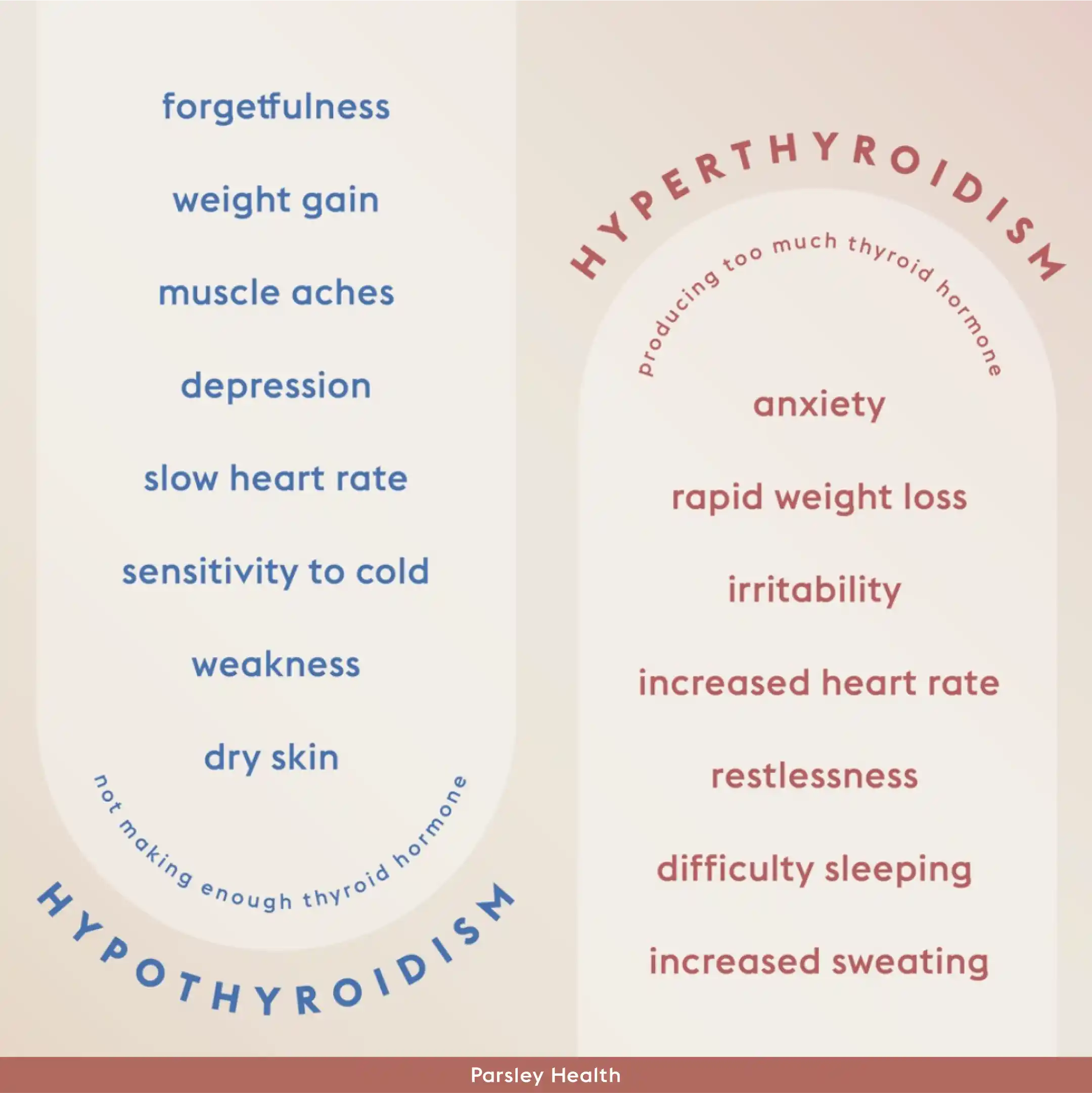
So, what does a Hashimoto's attack feel like? To start, these flare-ups lead to low levels of thyroid hormones. These hormones are essential for regulating your metabolism, body temp, heart rate, energy, menstrual cycle, mood, and hair and nail growth. When these hormones are out of whack, your body is, too.
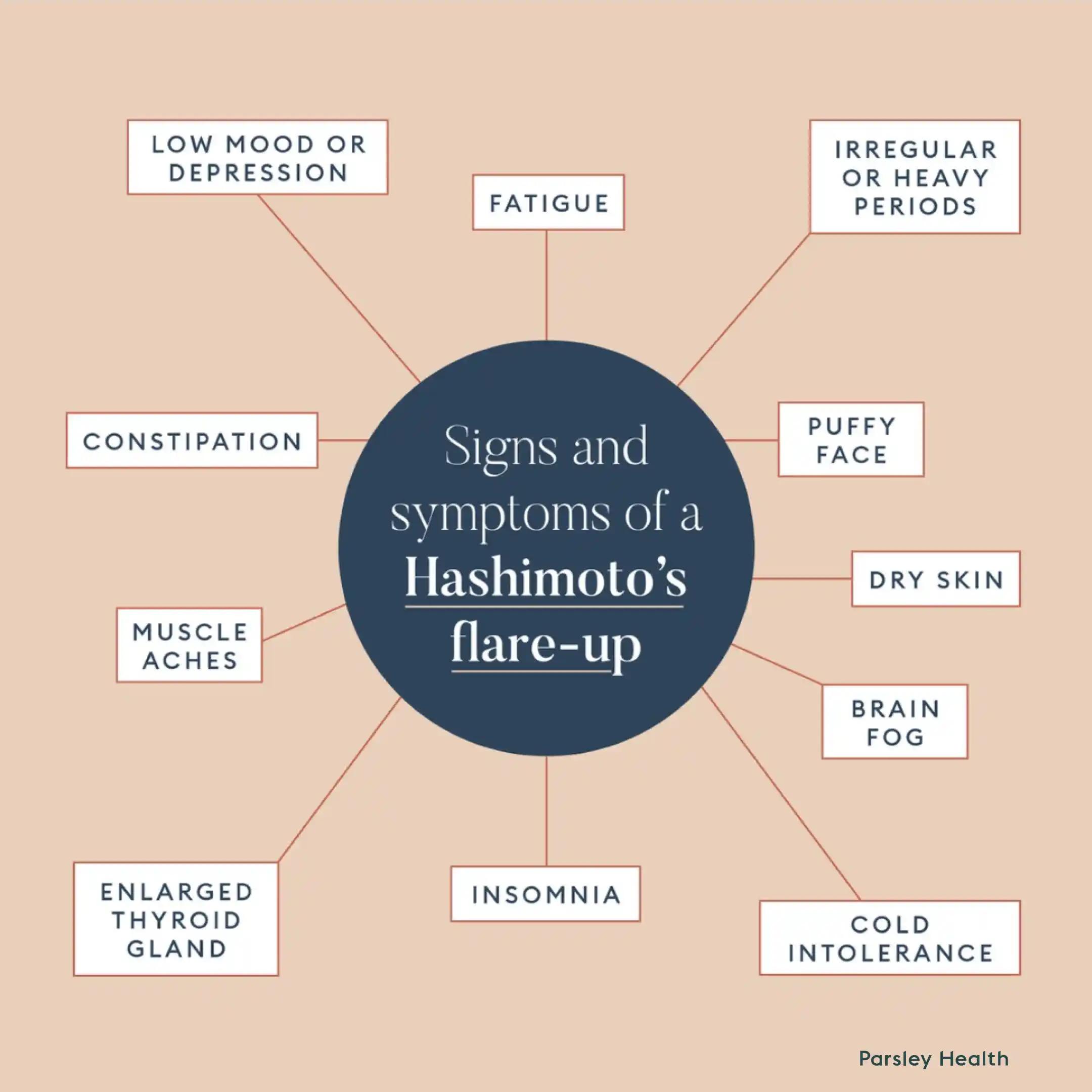
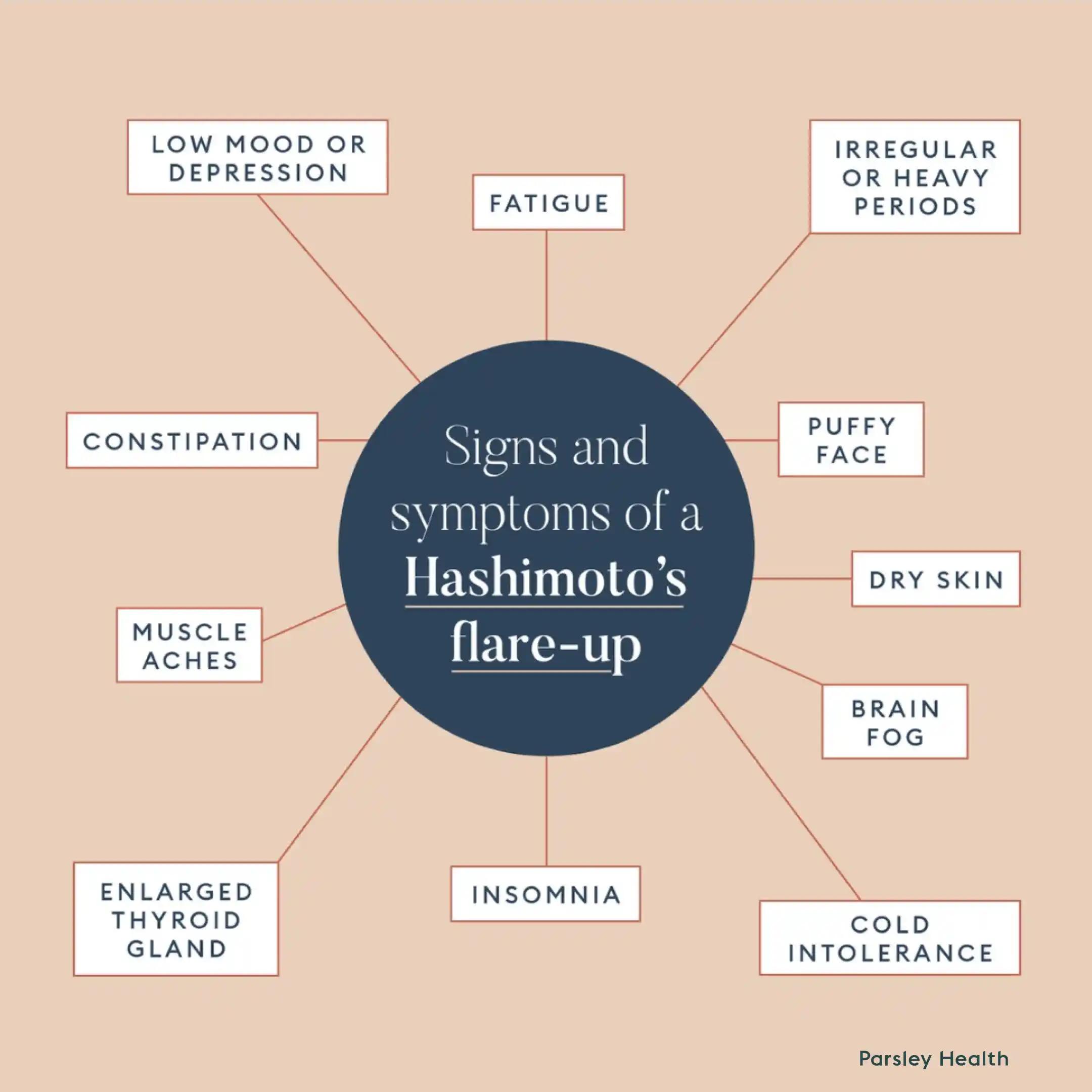 That means during a Hashimoto's flare-up you may feel fatigue, gain weight, be perpetually cold, experience constipation, have fertility issues, brain fog, or have aching joints and muscles. However, not all symptoms are present for everyone or in all flare-ups.
That means during a Hashimoto's flare-up you may feel fatigue, gain weight, be perpetually cold, experience constipation, have fertility issues, brain fog, or have aching joints and muscles. However, not all symptoms are present for everyone or in all flare-ups.
Not sure what your symptoms are really telling you?
The Parsley Symptom Index helps connect the dots across your whole body so you can understand patterns, not just isolated symptoms.
What are the symptoms of Hashimoto's disease flare up?
Hashimoto's symptoms can be vague. It’s easy to chalk them up to stressful weeks or lack of sleep, so you may not even notice there’s a problem at first. “Many people don’t know they have Hashimoto’s,” says Dr. Sharma. “They may know they have hypothyroidism, but doctor’s offices don’t frequently check for antibodies that signal an autoimmune condition,” she explains.
- Fatigue
- Cold intolerance
- Constipation
- Dry skin
- Puffy face
- Muscle aches
- Brain fog
- Insomnia
- Low mood or depression
- Irregular or heavy periods
- Migraines or headaches
- Enlarged thyroid gland (this is called a goiter)
Also be aware that it’s possible that a Hashimoto’s flare-up could cause your body to go into a hyperthyroid state, which means your thyroid is overactive. “With the destruction of thyroid cells, the gland releases thyroid hormones quickly into the bloodstream,” says Dr. Sharma. In that case, you can experience symptoms of hyperthyroidism, like:
- Fatigue
- Heat intolerance
- Irritability
- Rapid heartbeat
- Sleep problems
- Anxiety
 Risk Factors for Hashimoto's Disease
Risk Factors for Hashimoto's Disease
While it’s not entirely clear why people develop autoimmune conditions, Dr. Sharma says that it’s likely that you have a genetic predisposition to autoimmunity that’s activated by something in the environment. “Your immune system goes into dysfunction when the body is not in a healthy environment, and your thyroid tends to be the system that’s most responsive when things are off.”
But genetics don't act alone. For a Hashimoto's flare-up to occur, a trigger has to be present. “Each individual will have a unique immune system that responds differently to the environment. There is no one-size-fits-all when it comes to triggers,” explains Dr. Sharma.
However, there are some common lifestyle factors that may precede a flare and they fit in several larger buckets: diet, lifestyle, environmental, and medical. Knowing what they are can help you pinpoint the ones that are true to you:
- Your diet: According to Dr. Sharma, many people find that grains (specifically gluten -containing grains, like wheat, barley, or rye), high sodium intake, as well as high iodine intake are common triggers for a Hashimoto’s flare-up. Table salt is traditionally iodized, so if you’re eating a lot of high-salt foods you’re also likely consuming too much iodine.
- Your lifestyle: Lack of sleep or insomnia, high levels of stress, as well as being too sedentary—or conversely—overtraining with high-intensity exercise are triggers for flare-ups.
- The environment: Studies show that chemicals in plastics like bisphenol A (BPA), pesticide exposure, and air pollution, can disrupt thyroid function.
- Medical: There are pathogens like H pylori that can cause stomach ulcers are now known to be an easily overlooked trigger for Hashimoto's. An illness can also trigger the disease, as can hormonal fluctuations, which is one reason why the disease may disproportionately affect women.
Hashimoto's Diagnosis and Testing
Hashimoto's disease is diagnosed by a doctor who will examine your medical history and order a blood test. A simple blood test is essential because Hashimoto’s thyroiditis is a progressive disease. These antibodies will eventually damage and destroy your thyroid gland, even if symptoms of Hashimoto’s disease are not present now, says Dr. Sharma. “It helps to know if you have it so that you can do something about it early on and avoid the specific triggers that cause a flare,” she says.
If Hashimoto's is present, you don't have to figure out what to do alone. After a diagnosis, a doctor will work with you to create a treatment plan and should continue to monitor symptoms and triggers.
Healing stories from our members
Hashimoto’s Disease Treatment
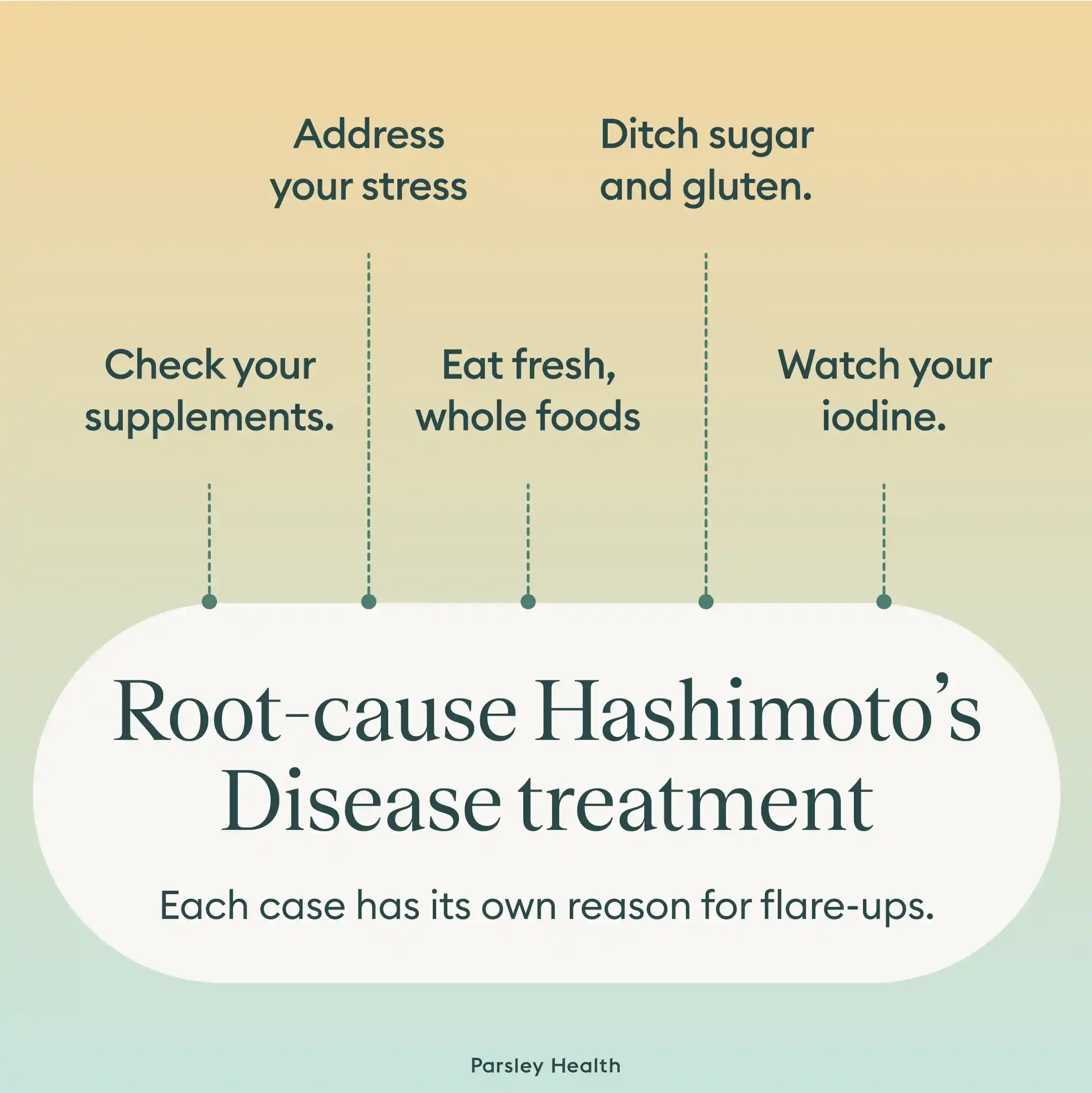
You’ll want to work with a doctor who can spend time with you to find what sets off your Hashimoto’s disease. “We have to figure out each individual’s reason for why they have these autoimmune antibodies in the first place,” says Dr. Sharma. Identify what might have happened in your life to lead to the flare, and then hone in on those factors to better manage symptoms throughout a flare—and help you feel your best. These are some ways Parsley Health’s doctors work with members to help them manage increased antibody formation and inflammation that leads to flares.
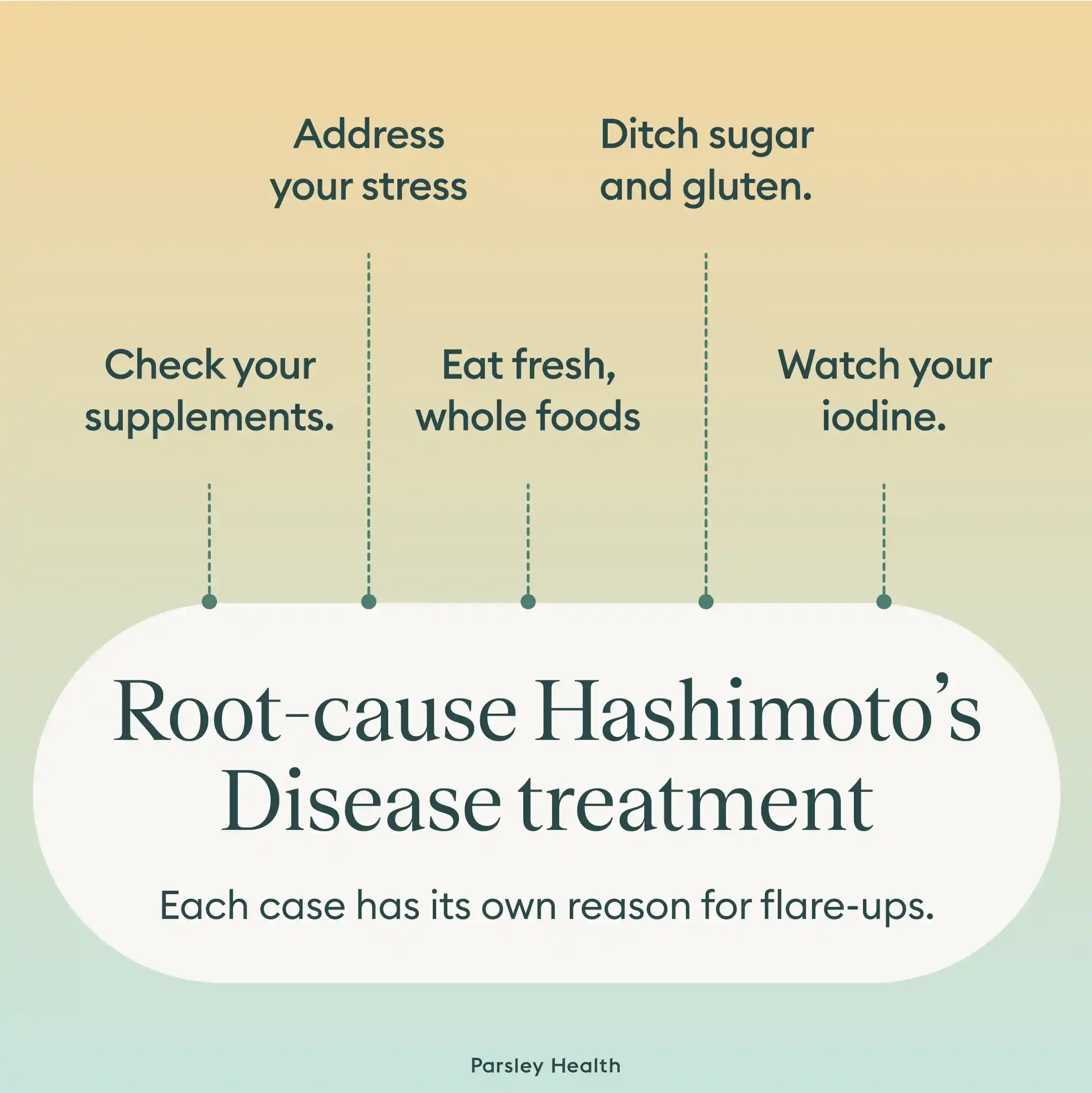 Address your stress.
Address your stress.
We all have stress, but when you have Hashimoto’s, it’s important to guard your time, give yourself some grace on your to-dos, and relax when you need it. It’s also important to realize that an overload of mental stress isn’t just a trigger for a flare itself, but can also impact your ability to care for yourself as you otherwise would, says Dr. Sharma. For instance, if you’re under stress, you might reach for less healthy foods or might be going to bed later or staying up late with worry and anxiety. Now is the time to go full-stop with self-care: unplugging when you need to/temporarily deleting social media apps, going to bed early, calling a friend to vent, and taking walks outside if you have the energy.
Check your supplements.
Is your body getting what it needs to fully support thyroid function? “We want to make sure that you’re supplemented enough with selenium and vitamin D in particular. You need all of the building blocks it takes to make thyroid hormone so that you’re not going into a hypothyroid state because of nutritional deficiencies,” says Dr. Sharma. We also want to make sure you are not getting excess iodine.
Eat fresh, whole foods.
Inflammation increases the autoimmune reaction, so focus on eating an anti-inflammatory diet, says Dr. Sharma. “Focus on non-processed foods, lots of vegetables and greens, organic meats, and reduce sugar intake,” she advises. Eat more dark leafy greens, which pack a powerful antioxidant called glutathione to help reduce inflammation, she says.
Ditch sugar and gluten.
Cookies and ice cream may be comforting in times of stress, but they’ll only exacerbate your symptoms now. Loading up your diet with sugar will lead to spikes and dips in blood sugar, something that activates your immune system, says Dr. Sharma. Since gluten is a trigger for many people, consider avoiding gluten-containing foods (many packaged snacks, wheat pasta, bread, cereal, and junk foods).
Watch your iodine.
Iodine is a mineral that your thyroid uses to make thyroid hormones. However, a high iodine intake, which can come from too much table salt (in the form of processed, packaged foods) will negatively affect thyroid functioning, says Dr. Sharma. She recommends sticking to a low-iodine diet during Hashimoto’s flare-ups.
What Causes a Hashimoto’s Disease Flare Ups?
A Hashimoto’s disease flare-up occurs when symptoms suddenly worsen or reappear after a period of relative stability. While flare-ups can feel unpredictable, they’re often triggered by a combination of immune, hormonal, and lifestyle factors rather than happening “out of the blue.”
Common triggers of Hashimoto’s flare-ups may include:
- Chronic or acute stress: Physical or emotional stress can influence immune activity and hormone signaling, potentially intensifying autoimmune responses and thyroid symptoms.
- Infections or illness: Viral or bacterial infections may temporarily activate the immune system, which can exacerbate autoimmune conditions like Hashimoto’s.
- Hormonal shifts: Changes related to menstruation, pregnancy, postpartum recovery, perimenopause, or menopause can affect thyroid hormone needs and symptom patterns.
- Nutrient deficiencies: Low levels of nutrients involved in thyroid and immune function, such as iodine, selenium, iron, vitamin D, or B vitamins, may contribute to symptom flares in some people.
- Digestive or gut health issues: Inflammation, food sensitivities, or changes in the gut microbiome may influence immune regulation and play a role in triggering flare-ups.
- Medication changes or inconsistent treatment: Adjustments to thyroid medication, missed doses, or changes in absorption can sometimes lead to symptom shifts.
- Poor sleep or overexertion: Inadequate rest or pushing through fatigue without recovery can make it harder for the body to maintain balance.
Not everyone with Hashimoto’s will experience flare-ups in the same way, or for the same reasons. Often, flares reflect a buildup of stressors rather than a single trigger. Identifying personal patterns can be a key part of managing symptoms more effectively over time.
Parsley Health offers physician-led functional medicine care, advanced lab programs, and flexible ways to get started, all designed to help you feel better over time.
Treatment Options for a Hashimoto’s Disease Flare Up
Managing a Hashimoto’s flare-up typically focuses on calming symptoms, supporting thyroid function, and addressing the underlying factors that may have contributed to the flare, rather than chasing quick fixes.
Treatment approaches may include a combination of the following:
Medication management
For many people with Hashimoto’s, thyroid hormone replacement is an essential part of treatment. During a flare-up, symptoms may signal that thyroid levels need to be re-evaluated. Any medication adjustments should always be guided by a licensed clinician and appropriate lab testing.
Stress reduction and nervous system support
Because stress can significantly influence autoimmune activity, prioritizing rest, gentle movement, and stress-management practices may help shorten or soften flare-ups. This can include breathing exercises, mindfulness, pacing daily activities, or simply allowing for more recovery time.
Nutrition and inflammation support
A nutrient-dense, anti-inflammatory eating pattern may help support immune balance during a flare. Some people benefit from temporarily avoiding foods that seem to worsen symptoms, while focusing on adequate protein, healthy fats, and micronutrients important for thyroid health.
Addressing nutrient deficiencies
If deficiencies are present, correcting them under medical guidance may support thyroid function and overall energy levels. This often requires testing rather than guessing.
Supporting gut health
Because the gut and immune system are closely connected, addressing digestive symptoms or underlying gut issues may be part of a longer-term strategy to reduce flare frequency.
Personalized, root-cause care
Rather than treating flare-ups as isolated events, a whole-body approach looks at why they’re happening in the first place. Parsley Health clinicians often evaluate hormone balance, stress physiology, nutrient status, and lifestyle factors together to help reduce the likelihood of recurring flares.
Everyone’s experience with Hashimoto’s is different. While flare-ups can be discouraging, they can also provide valuable information about what your body needs more, or less, of at a given time.
When to See a Doctor
As soon as symptoms appear, see a doctor about Hashimoto's disease. While this condition often progresses slowly, early diagnosis and developing a robust treatment plan can prevent future flare-ups. Since the disease has a genetic component, it's also best to bring up Hashimoto's with a doctor if there's a family history of thyroid disease.
To make your time at the doctor's meaningful, consider asking:
- What Hashimoto's triggers should I be looking for?
- Are there any lifestyle adjustments I can make to avoid future flare-ups?
- What symptoms might I experience, and what should I do if I experience them?
- When should I schedule a follow-up appointment?
Frequently asked questions about Hashimoto’s Disease Flare Ups
What are the worst symptoms of Hashimoto's?
The worst symptoms of Hashimoto's can vary from person to person since "worst" is subjective. That being said, some of the symptoms that cause the most complications or disruption to daily life include fatigue, depression, muscle aches, brain fog, and rapid heartbeat.
What aggravates Hashimoto's?
Environmental triggers aggravate Hashimoto's and can cause a flare-up. Triggers differ from person to person, but some of the most common include processed foods, sugar, gluten, lack of sleep, and a sedentary lifestyle.
What are Hashimoto's inflammatory attacks?
Hashimoto's inflammatory attacks occur when symptoms intensify or are made worse, usually due to an environmental trigger like sugar or exposure to pesticides. Because attacks are marked by a sudden and swift return (or increased severity) of symptoms, they are also called flare-ups.
How does a person with Hashimoto's feel?
Hashimoto's disease looks different for everyone, but some common symptoms include fatigue, brain fog, muscle aches, and constipation. The disease can also impact how you feel mentally, and it has been linked to depression and anxiety. Additionally, many with Hashimoto's suffer from insomnia or trouble sleeping.
Final Thoughts
When a Hashimoto attack occurs, it can interrupt your day-to-day life and leave you feeling drained emotionally and physically. Fortunately, flare-up triggers and symptoms can be managed, often with the help of a trusted physician. Contact Parsley Health for more insight on how to control and prevent Hashimoto's flare-ups.
 That means during a Hashimoto's flare-up you may feel fatigue, gain weight, be perpetually cold, experience constipation, have fertility issues, brain fog, or have aching joints and muscles. However, not all symptoms are present for everyone or in all flare-ups.
That means during a Hashimoto's flare-up you may feel fatigue, gain weight, be perpetually cold, experience constipation, have fertility issues, brain fog, or have aching joints and muscles. However, not all symptoms are present for everyone or in all flare-ups.


 Risk Factors for Hashimoto's Disease
Risk Factors for Hashimoto's Disease




 Address your stress.
Address your stress.