This article was medically reviewed by Nisha Chellam, MD. It contains additional reporting by Angela Myers.
Did you know you actually have a chill-out button in your back pocket? It’s called the vagus nerve. (And, yes, vagus nerve exercises are a thing.)
“The vagus nerve connects the brain to the body, and its primary function is to activate our parasympathetic nervous system (PNS),” says Erin D’Elia Assenza, a certified health coach at Parsley Health. There are two branches of the autonomic nervous system or peripheral nervous system (PNS), or “rest and digest” and sympathetic nervous system (SNS), or “fight and flight.”
Of course, it’s not literally located in your back pocket—the vagus nerve runs from the brainstem through the neck and down to your abdomen. Its main function is to regulate digestion and your heart and breathing rate. When it’s activated, it will temper your physiological stress response, allowing a feeling of calm to wash over you. And the good news? There are specific exercises you can do for vagus nerve stimulation.
Common problems related to the vagus nerve
Running from the brain and cranial nerves to the large intestines, the vagus nerve impacts various physical and psychological functions. And with all those connections, an irritated vagus nerve can cause a few problems.
The vagus nerve modulates the parasympathetic nervous system, a part of the brain that controls stress and emotional reactions. When the vagus nerve isn't working properly, neither is that part of the brain, causing mood problems and a rise in stress hormones. In fact, one 2020 study linked irritations in this nerve to depression, anxiety, and PTSD—and found vagus nerve stimulation can decrease these conditions.
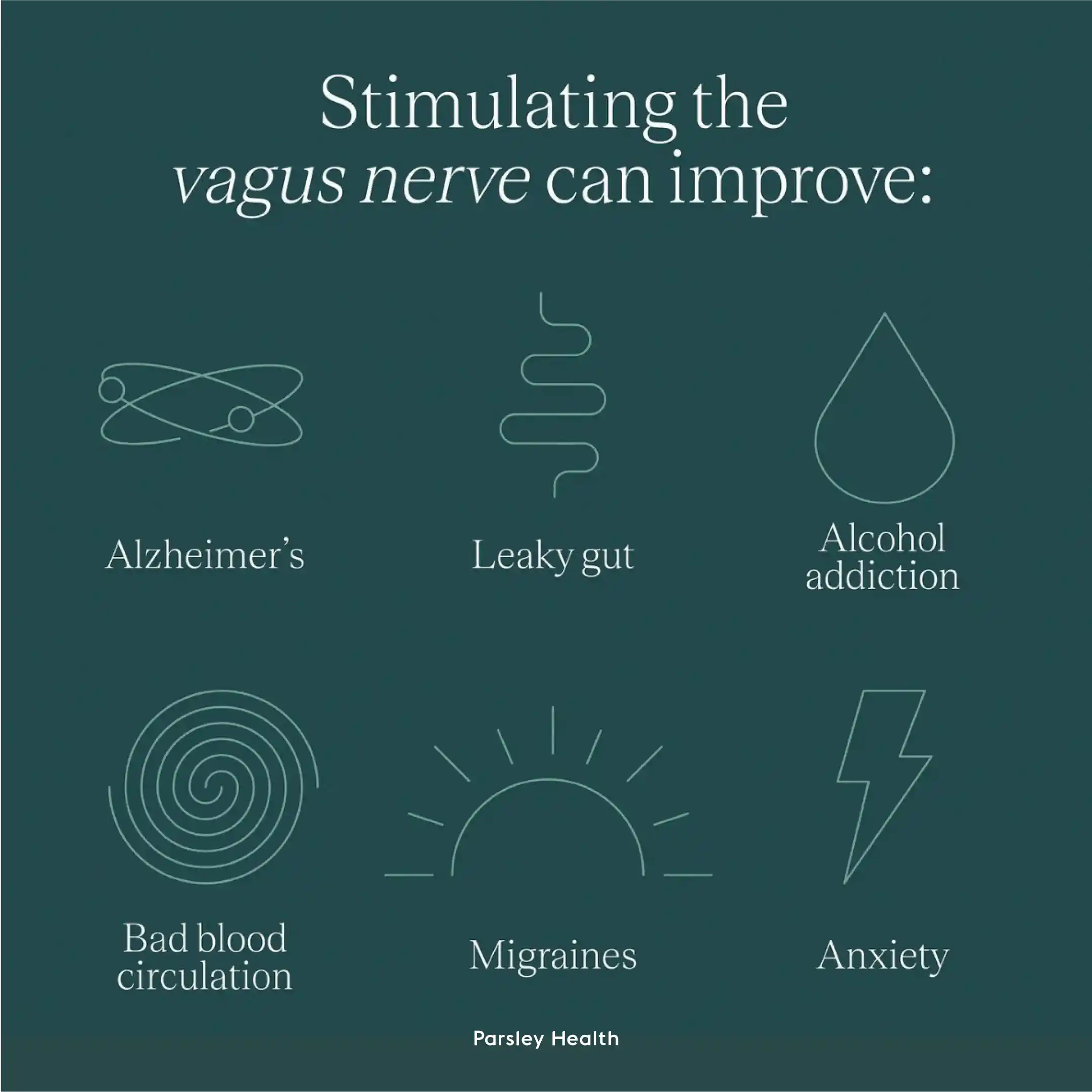
Thanks to its crucial placement, the vagus nerve is also a channel that receives signals from the gut microbiota and zips that info over to the brain, notes a 2018 paper in Frontiers in Neuroscience. The authors point out that stress inhibits the vagus nerve and may be linked to GI disorders like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) through inflammation.
When to stimulate the vagus nerve
It’s an impossible game to try to avoid stress. Since stress is ubiquitous, it’s how you react to it that counts the most when it comes to your wellbeing. So vagus nerve stimulation can be a tool you use during any moment you need to de-stress.
“Stimulating the vagus nerve tricks your brain into thinking that everything is okay,” says D’Elia Assenza. A great time to stimulate the vagus nerve, she says, is when experiencing a heightened state of anxiety or stress situations. “When something feels out of your control, these exercises are something you can do that’s in your control,” says D’Elia Assenza. You can also practice vagus nerve exercises regularly to better build up your resilience against stress. “I believe we should prioritize our stress every day—even when we don’t feel like we’re stressed. It’s such a huge part of having optimal health,” she says.
Benefits of vagus nerve stimulation
Consider what happens when your sympathetic nervous system is keyed up —maybe you’re stuck in traffic, just received a nasty email, feel overwhelmed at your job, or had a fight with your partner or a friend. “When you’re in fight-or-flight mode, the job of the SNS is to promote survival. So, in the face of a threat, your body wants to make sure you can run for your life: Your heart rate increases, your pupils dilate, and other systems you don’t need at the moment are down-regulated. Meaning digestion, immune, and reproductive systems slow,” says D’Elia Assenza. When you employ vagus nerve exercises that tell your brain and body that all is well, you not only can tap into a better headspace, but your physical health benefits, too.
In essence, the vagus nerve plays an important role in the gut-brain axis, which affects your mood and has been implicated in then development of depression and anxiety.
Another study, published in the same journal, noted that vagus nerve stimulation may be an additional therapy for treatment-resistant depression and posttraumatic stress disorder. (Of course, these exercises are not a substitute for treatment your provider has recommended for you.)
Doing vagus nerve exercises also increases your vagal tone, which D’Elia Assenza describes as your capacity to handle stress and determines how quickly you can bounce back from stressful events. “Think of it like exercise—you may stimulate your ab muscles by doing crunches to have greater muscle tone in your core,” she says.
Should you try vagus nerve exercises?
There are so many ways you can stimulate the vagus nerve—and they can be fun, calming, or fit in with the day-to-day routines you already have in place. “The list of things you can do is extensive. You don’t have to do them all, you can choose the activities that you like and make you feel good,” D’Elia Assenza says.
She likes to break them up into two categories: physical and emotional vagus nerve stimulators and encourages clients to look at them as a toolbox. You can pick out the ones you need in the moment or that resonate with you at that time. Aim to get in five minutes a day, throughout the day of the below vagus nerve exercises.
Physical vagus nerve exercises
These activities all center around one thing: Manipulating the vocal cord. “The physical reverberation of your vocal cords can activate the vagus nerve,” D’Elia Assenza explains.
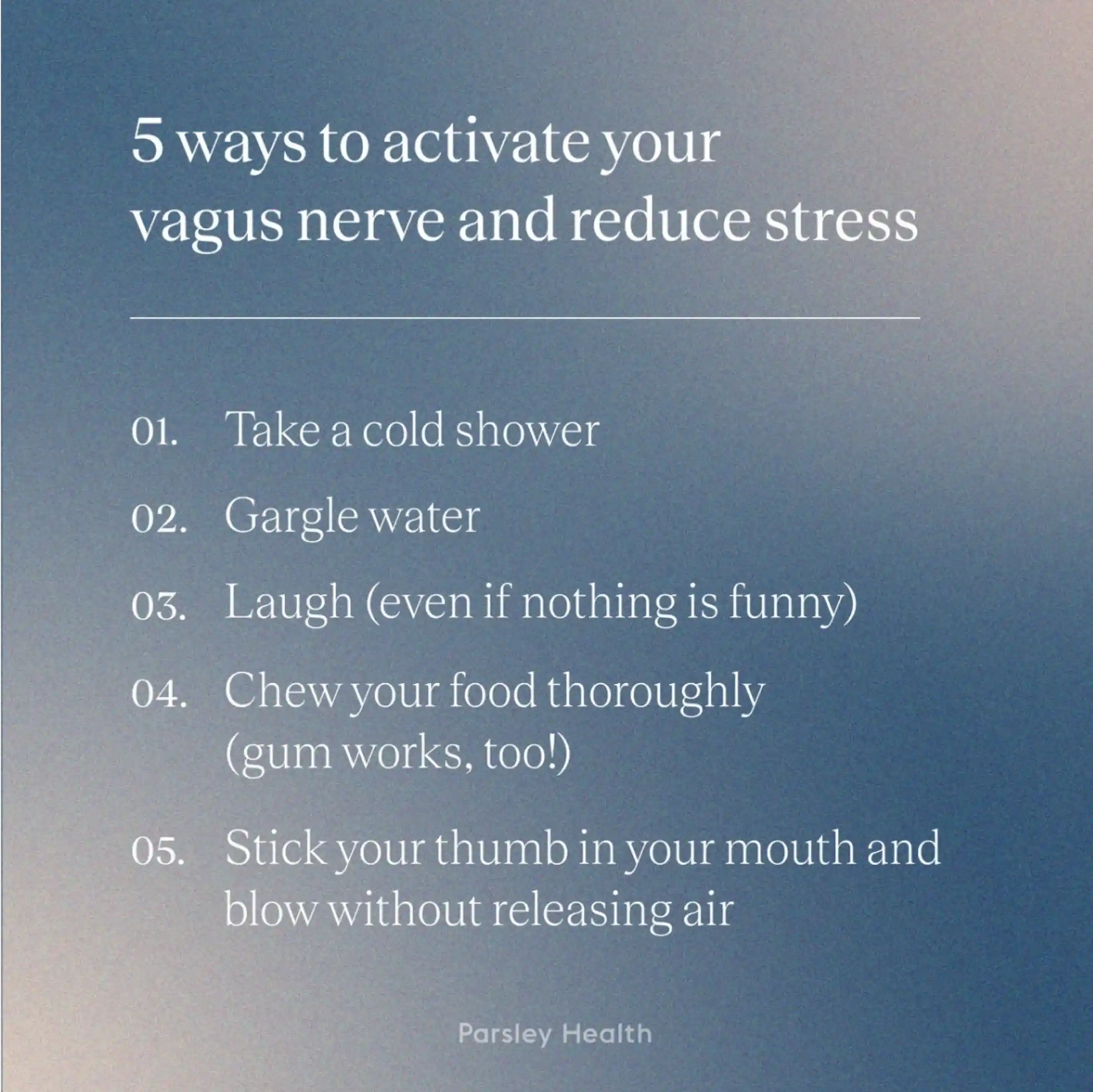
Gargling
Gargle with water in the morning and evening when you brush your teeth. Aim for 30 seconds to one minute. This is a great way to calm the vagus nerve since the throat is engaged in gargling.
Singing
Doesn’t matter if you can carry a tune (or make dogs howl with your pitch), turn on your favorite song and belt it out. Interestingly, the slower you sing, the better it is for your vagus nerve. A 2022 study found slow, controlled singing positiveely impacted overall stress levels and the vagus nerve.
Om-ing
Yes, the same om associated with yoga practice . Sitting in a quiet space, chant a long “om.” You should feel a vibration around the ears, which will connect to the vagus nerve. A study in the International Journal of Yoga found that chanting ‘om’ was helpful in deactivating certain parts of the limbic system in the brain involved in stress and emotional responses, such as the amygdala.
Laughing
Watch a funny TV show or movie and actually LOL at the funny parts. Or, get together with that friend who you always get slapstick-happy with to get in an extra good guffaw. A 2022 study outlined laughter's various benefits, including calming the vagus nerve.
Psychological vagus nerve exercises
Getting the vagus nerve moving isn’t the only way to stimulate the vagus nerve though—your thoughts and feelings can activate it, too. “Eliciting an emotional response that can be supportive to the vagus nerve and calming parasympathetic nervous system,” says D’Elia Assenza.
Gratitude Journaling
Sit down before bed or when you wake up and write down three things you’re grateful for, whether they’re big (your family) or small (that nourishing oat milk latte this morning). Repeat this daily, weekly, or a cadence that feels right for you to help activate the PNS.
Deep breathing
The Box Breath is one breathing exercise that D’Elia Assenza likes. (Also called a square breath.) Inhale for a count of 4, hold for a count of 4, exhale for a count of 4, hold for a count of 4. Repeat as many times as you need. Deep breathing tricks your body into thinking, “I can’t possibly be running for my life if I’m breathing this slowly.”
Meditating
Meditating can take many forms and does not have to be long and drawn out, but “contemplative practices,” such as meditation and yoga, have been found to bring calm, in part, by activating the vagus nerve, according to research. Spend five minutes on an app like Headspace, Calm, or Insight Timer for short guided meditations.
Nature exposure
Exposing yourself to things that are beautiful, such as a sunset, spending time in nature , looking at pretty pictures, or playing with your pets. Anything that brings forth positive emotions—and this is different for everyone—increase vagal tone, and has been found to be a contributor to good physical health, notes a randomized controlled trial in Psychological Science.
Commonly Asked Questions
What is the fastest way to calm the vagus nerve?
The quickest way to calm the vagus nerve is to splash cold water on the face. Other speedy tricks include breathing slowly, doing a short meditation, and laughing. Om-ing or singing can also help.
What are the symptoms of an irritated vagus nerve?
An irritated vagus nerve can cause impact your body's digestive tract, muscus and saliva production, taste, and speech. Thanks to its role connecting the brain and gut, this nerve can also cause psychological symptoms. A 2018 study, for example, linked an irritated vagus nerve to anxiety, depression, and a negative mood.
What exercise is best for the vagus nerve?
Often, the best "workout routine" for the vagus nerve includes physical and psychological exercises. Great physical exercises include gargling, singing, om-ing, and laughing. Some psychological vagus nerve exercises are deep breathing, gratitude journaling, and meditation.
Where is the pressure point for the vagus nerve?
There isn't one "pressure point" for the vagus nerve. Instead, various pressure points on the neck and ear can impact the vagus nerve. To massage these pressure points, gently rub the top of your earlobe, the base where your ear and jaw connect, and along your neck.

