Ulcerative colitis (UC) is an inflammatory bowel disease that causes uncomfortable gastrointestinal symptoms, like diarrhea and rectal bleeding, and can impact overall health. Despite UC’s symptoms and rising prevalence, it’s often underdiagnosed. Here are the ulcerative colitis symptoms to watch out for and how a functional medicine approach can help detect and treat UC.
About 600,000 to 900,000 Americans in the US have ulcerative colitis, though that stat only encompasses those with an official diagnosis. While the condition is common, it’s often underdiagnosed, especially in women.
But what exactly is ulcerative colitis — and how do you know if you need to see a doctor about it? UC is a type of inflammatory bowel disease and an autoimmune condition that impacts the digestive tract. Continue reading for quick refresher on UC and a detailed look at symptoms to watch out for, when to see a healthcare provider, and treatment options.
Understanding ulcerative colitis
“Ulcerative colitis is a chronic inflammatory bowel disease with inflammation and ulcers (sores) in the lining of the colon and rectum,” explains David Clarke, MD, a board-certified gastroenterologist and President of the Association for the Treatment of Neuroplastic Symptoms. The inflammation and sores disrupt the digestive process, often resulting in diarrhea (too frequent bowel movements) and blood in stool, among other symptoms.
To fully understand ulcerative colitis, we need to examine the colon and rectum, two key parts of the digestive tract that regulate bowel movements. The colon is a tube-shaped part of the large intestine that connects the small intestine to the anus and rectum.
As food and liquids make their way down the digestive tract, the colon extracts important nutrients and electrolytes that the body can use before transporting the leftover waste, called stool, to the rectum and anus, where it leaves the body.
“Ulcerative colitis is an autoimmune condition, meaning the immune system mistakenly attacks the cells of the colon, leading to ongoing inflammation in the colon and rectum,” explains Dr. Clarke. That inflammation then causes the colon walls to weaken, leading to disruptions in the digestive process.
Not sure what your symptoms are really telling you?
The Parsley Symptom Index helps connect the dots across your whole body so you can understand patterns, not just isolated symptoms.
Common symptoms of ulcerative colitis
As you may have guessed, ulcerative colitis’ most common symptoms affect the gastrointestinal tract. They include stomach pain, diarrhea, more frequent or urgent bowel movements, rectal bleeding, and blood in stool.
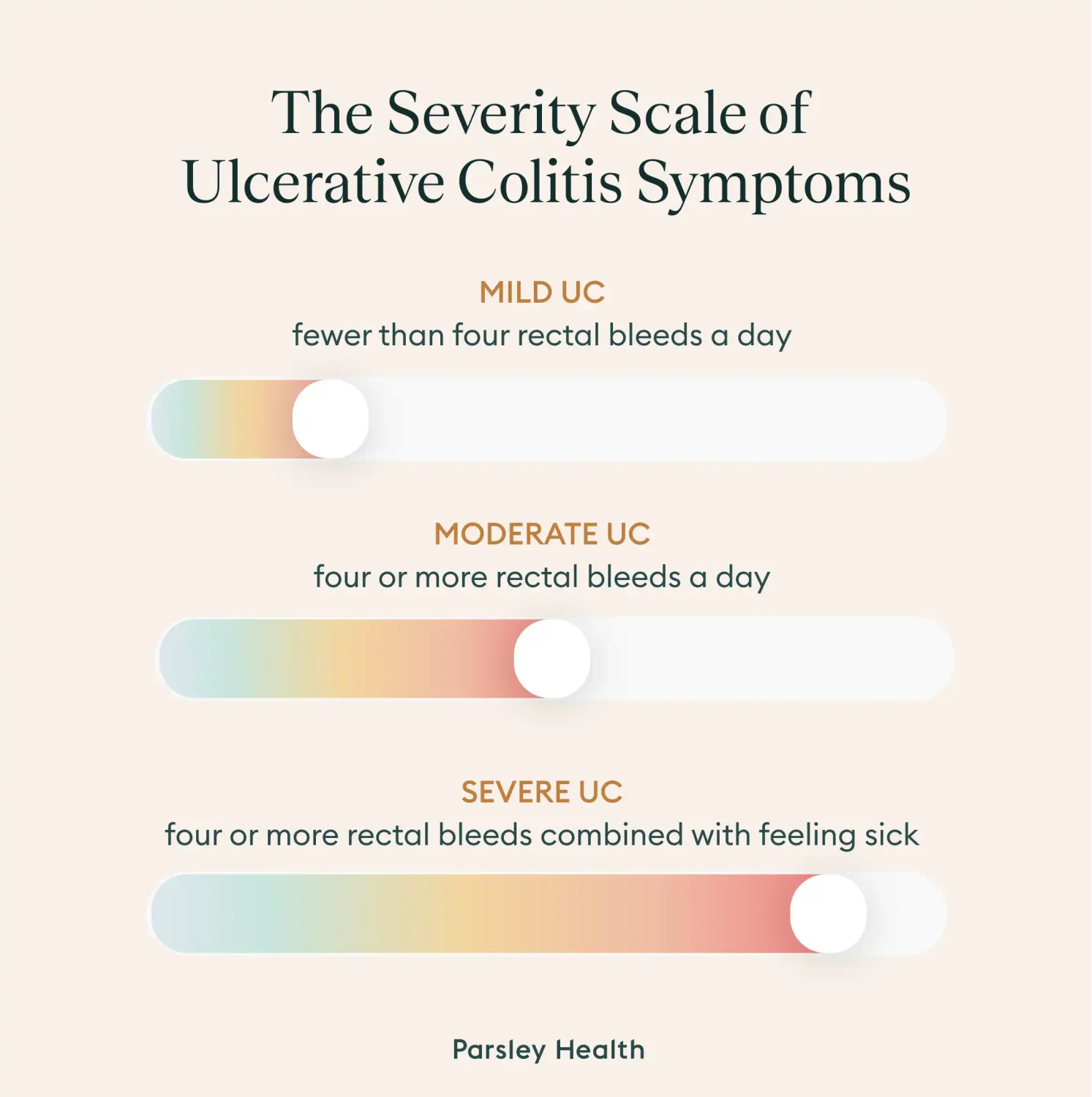
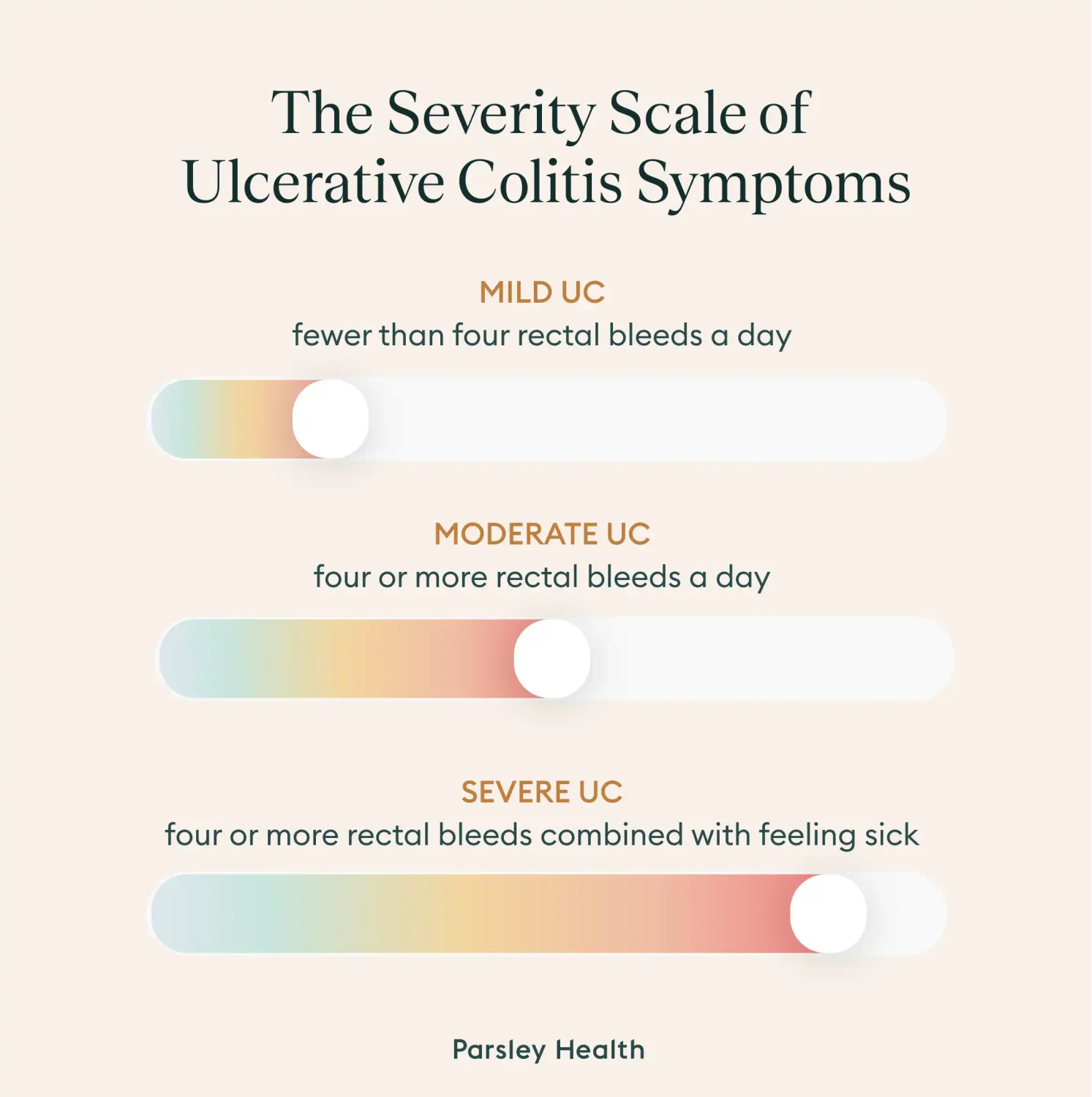
The severity of UC is often determined by the frequency of rectal bleeding:
- Mild UC: When there’s fewer than four rectal bleeds a day.
- Moderate UC: When there’s more than four daily rectal bleeds without other symptoms
- Severe UC: When there’s four or more rectal bleeds combined with feeling sick (fatigued, running a fever, severe stomach cramping) or not getting enough albumin, a protein required for normal kidney and GI tract function
The gut is referred to as our second brain for a reason; it communicates and provides essential nutrients to many other parts of the body. UC’s symptoms disrupt normal communication between the gut and other parts of the body. And when UC causes diarrhea, food and water often leave the GI tract before the body can get essential nutrients for optimal health.
A lack of essential nutrients and disrupted communication from the gut often results in extra-intestinal symptoms, such as:
- Joint pain
- Fatigue
- Loss of appetite
- Unintended weight loss
- Rashes or sores on skin
UC also increases the chance of other medical conditions such as anemia, a dangerous loss of iron required for oxygen production, pelvic abscess, a life-threatening collection of pus in the pelvis, and toxic megacolon, a rare and life-threatening infection of the colon. Those with UC are also two to three times more likely to develop colon cancer.
What causes ulcerative colitis?
“The fundamental cause is not fully understood, but genetic, immune, and environmental factors are believed to contribute,” says Dr. Clarke, “Ulcerative colitis is most common in young adults, affects both sexes and is more prevalent in white Americans and those of Ashkenazi Jewish descent, with family history being a major risk factor.”
In fact, over 200 different genes impact someone’s risk of getting UC, and if an immediate family member has the condition, you’re more likely to develop UC.
But ulcerative colitis isn’t just a genetic disease; environment and diet are to blame as well. Since UC is an inflammatory condition, eating inflammatory foods (think: highly processed foods like cakes, chips, and hot dogs) increases the risk, especially if someone is already genetically predisposed. Environmental pollutants may also play a role since the rate of UC is higher in industrialized areas.
How ulcerative colitis is diagnosed
To diagnose ulcerative colitis, a doctor will start by reviewing a patient’s medical and family history, as well as performing a physical exam. Additional tests are also required, including:
- Blood tests
- Stool tests
- An endoscopy of the large intestine, usually a colonoscopy, where a doctor investigates the rectum and colon with a colonoscope, or a flexible sigmoidoscopy, where the doctor investigates the colon and rectum with a sigmoidoscope
While these tests determine if ulcerative colitis is present, they don’t provide an overview of the individual’s overall health. Since UC flares may stem from diet, lifestyle, and stress, it’s important to get that full picture. A functional medicine provider will order additional tests to assess nutrition and lifestyle and provide a whole-person treatment plan.
Healing stories from our members
Integrative treatment approaches
Treatment for UC is twofold: calming any flares and preventing future ones. Both can be tackled through an integrative treatment approach that balances nutrition, lifestyle changes, and medical support.
Below, we’ve outlined the most common types of treatment, but it’s important to remember that the right mix of treatments differs.“Everyone’s UC is different,” explains Dr. Clarke, “so what works for one person may not work for another. It’s important to understand your own triggers and tolerances.”
Diet and nutrition
Diet plays an important role in ulcerative colitis. During a flare, you want to avoid any trigger foods. “Be mindful of common UC trigger foods such as high-fiber items, spicy foods, caffeine, and alcohol,” explains Dr. Clarke, “These can vary from person to person, so stick to what you know works for you.” Some flare–friendly snacks Dr. Clarke often recommends to patients are crackers, bananas, and applesauce.
When symptoms aren’t flaring, stick to an anti-inflammatory diet that helps keep your gut healthy and immune system in check. Research suggests the Mediterranean diet may be the best for UC.
This diet, which is for periods of remissions and not UC flares, focuses on eating plenty of:
- Leafy greens
- Fruits
- Whole grains
- Nuts
- Legumes, like lentils or chickpeas
- Olive oil
- Low amounts of cheese and yogurt
- Fish or lean meat, eaten a few times a week
- Small amounts of wine consumed with a meal
For the Mediterranean diet, it’s best to avoid red meat, large amounts of dairy, and sugary or ultra-processed foods. Those with ulcerative colitis often benefit from working with a functional medicine provider and/or dietitian to identify any other personal triggers to avoid.
Gut health support and supplements
Eating an anti-inflammatory diet is a great start at reducing inflammation, but it’s also important to do a quick gut check. UC is associated with an imbalance of microbiota in the gut. By strengthening good gut bacteria, someone may be able to help reduce UC flares.
In fact, individuals with UC often have higher remission rates after introducing a probiotic, a dietary supplement that supports good gut microbiota, into their diet.
A small-scale study even suggests specific microbiota strains that can help, especially with mild to moderate UC cases: prausnitzii and lactobacilli. Both can be found in various fruits and veggies, as well as select probiotics. For a recommendation on a probiotic for UC, consult a functional medicine provider.
While probiotics are effective, a functional healthcare provider should first test the gut to make sure it is ready before someone starts a probiotic. If the gut isn’t ready, the probiotic won’t work as intended, so testing and professional guidance is key.
Lifestyle and stress management
What you put on your plate isn’t the only lifestyle choice that matters; stress, a sedentary lifestyle, and chronic poor sleep can also increase the likelihood and severity of UC flares. While none of these directly affect UC, they all influence the immune system and gut health.
Lifestyle modifications that may help include:
- Workout regularly: Both high intensity workouts (i.e. CrossFit, powerlifting, and running) and low intensity workouts (i..e yoga, pilates, walking) help. The key is to stay consistent.
- Practice good sleep hygiene: Think sleeping in a dark, cool room, avoiding screens 30 minutes before bed, and having a calming nighttime routine, such as taking a hot bath or reading a book.
- Integrate stress management practices into your daily life: GI-focused meditations and breathwork, such as boxed breathing, are evidence-based practices to start with.
Medications
When symptoms are severe, a doctor may recommend prescription medications. These medicines can help reduce flares, though they don’t “cure” ulcerative colitis. The most common include:
- Aminosalicylates (5-ASA): Control mild to moderate symptoms and are often seen as the first line of pharmaceutical defense.
- Corticosteroids: Taken during a moderate to severe flare, but shouldn’t be used indefinitely due to side effects of long-term use, such as vision problems and high blood pressure.
- Immunomodulators: A class of medication that suppresses immune responses. They’re often prescribed for patients with severe flares.
- Biologics and small molecule drugs: When other treatments fail, a doctor may recommend either of these two drug classes.
If UC isn’t responding to medication or there’s complications, like colon cancer, surgery may be recommended. “Surgical options include total colectomy, the removal of the colon, with or without creation of an ileal pouch-anal anastomosis,” adds Dr. Clarke.
Key takeaways
Whether you’re curious about if you have ulcerative colitis or looking for a better way to manage symptoms, keep in mind:
- Ulcerative colitis is an autoimmune condition and an inflammatory bowel disease that causes ulcers in the rectal lining and colon.
- UC is a life-long condition, meaning it can’t be cured. It is possible to reduce flares and prolong remission periods through an integrative treatment approach that incorporates an anti-inflammatory diet, gut health support, stress reduction, good sleep hygiene, and regular exercise. In moderate to severe cases, medication may also be recommended.
- A functional medicine provider like Parsley Health can help manage UC flares, creating long-lasting change.
Parsley Health offers physician-led functional medicine care, advanced lab programs, and flexible ways to get started, all designed to help you feel better over time.
Frequently asked questions (FAQs)
Does ulcerative colitis go away on its own?
While ulcerative colitis goes through periods of remission where there’s no symptoms, and flares where there are symptoms, it never completely goes away. It’s a lifelong condition that can be managed through dietary and lifestyle modifications, sometimes alongside medication or surgery.
What is the life expectancy of someone with ulcerative colitis?
Those with ulcerative colitis have a normal life expectancy. That said, there are some life-threatening complications associated with UC, highlighting a need to manage symptoms.
What triggers ulcerative colitis?
UC flares are often triggered by specific foods, periods with little exercise and movement, stress, and poor gut health.
What are the early warning signs of ulcerative colitis?
Gastrointestinal symptoms, such as recurring diarrhea and stomach pain, are often the first warning signs of ulcerative colitis.
Can I live a normal life with ulcerative colitis?
Many people with ulcerative colitis live a normal life. So long as symptoms are managed, someone can have a relatively high quality of life, especially during periods of remission, and an average life expectancy.
How serious is ulcerative colitis?
Ulcerative colitis can cause serious, life-threatening complications and increases the risk of colon cancer. As a result, it’s important to work with a doctor, such as a functional medicine provider or gastroenterologist, to manage symptoms.
What is the difference between colitis and ulcerative colitis?
Colitis is a general term referring to inflammation in the colon. Ulcerative colitis is a specific type of colitis that leads to ulcers in the colon, resulting in diarrhea, blood in stool, and rectal bleeding.