This article has been medically reviewed by Nisha Chellam, MD. It contains additional reporting by Jennifer Chesak.
SIFO symptoms can have you running for the bathroom, doubling over in discomfort, or reaching for a pair of looser pants.
The acronym stands for small intestinal fung al overgrowth, which can cause uncomfortable bloating, abdominal pain, and diarrhea.
You may have heard of its cousin SIBO, which stands for small intestinal bacterial overgrowth. However these conditions have key differences, and they don’t necessarily respond to the same treatments.
Keep reading to get the rundown on SIFO, which could be the underlying cause of your digestive symptoms.
What is SIFO?
“SIFO is essentially fungal overgrowth in the small bowel (or small intestines), as opposed to the bacterial overgrowth that occurs in SIBO,” says Sarah Steinberg, MD, PhD, a double-board certified internal medicine and gastroenterology physician.
The most common fungus associated with SIFO is some form of candida, such as Candida albicans. Candida is a member of the fungal family, but it is typically referred to as a yeast.
Candida normally lives on the skin and inside the body—in places like the mouth, throat, gut, and vagina—without causing problems.
“But, like anything else in the gut, when [candida] gets really out of balance, that’s when it becomes an issue,” Steinberg says.
A variety of factors, from diet to low stomach acid to certain medications, may contribute to fungal overgrowth in the gut.
Candida overgrowth can take place in other areas of the body, too—learn how it can affect the health of your skin and nails, vagina, mood, and more.
What are common SIFO symptoms?
In one small study of 150 people with unexplained GI issues, around 25 percent had SIFO.
Their most common symptoms were the following:
belching
bloating
indigestion
nausea
diarrhea
“The most common symptoms of SIFO are really the same as those for SIBO,” Steinberg says. “But my red flags for SIFO go up when I see other signs of fungal overgrowth, such as chronic yeast infections or rashes in areas where skin meets skin, like armpits or under the breasts. Some patients also experience itching behind the ears.”
Toenail fungus, anal itching, and oral thrush may also be indicators that you have some sort of systemic fungal overgrowth occurring. Oral thrush is candida overgrowth in the mouth and usually presents as a white coating on the tongue.
These non-GI symptoms aren’t always present in people with SIFO. However, they may prompt your provider to investigate further.
“If there is fungal overgrowth in other places, it makes me think there may be fungal overgrowth in your gut as well,” Steinberg says.
What are the major SIFO risk factors?
SIFO may be behind your GI symptoms. However, what's leading to SIFO in the first place? Several root causes can encourage unhealthy growth of fungi. According to Dr. Steinberg, the following are some of the most common factors.
You’re immunocompromised
Overgrowth of fungi is often more common in people with weakened immune systems. You may have a weakened immune system and be more susceptible to SIFO for these reasons.
You have HIV, cancer, diabetes, or an autoimmune disease
You take or have recently taken immunosuppressant drugs, steroids, or antibiotics
You've been hospitalized
You've had an organ transplant
Children and seniors are also more likely to develop SIFO than people in other age groups, and this may be related to their immune system status.
You’ve used proton pump inhibitors (PPIs)
Proton pump inhibitors (PPIs) are medications commonly prescribed for acid reflux. They work by reducing how much acid that the glands in your stomach produce.
However, a certain level of stomach acid is needed for digesting food and killing potentially harmful microbes before they reach the intestines.
Long-term use of these medications has been implicated in both SIFO and SIBO.
You have low stomach acid levels
In addition to long-term PPI use, a variety of factors, such as age, nutrient deficiencies, and underlying conditions, can contribute to low stomach acid levels, which may make you more likely to develop SIFO.
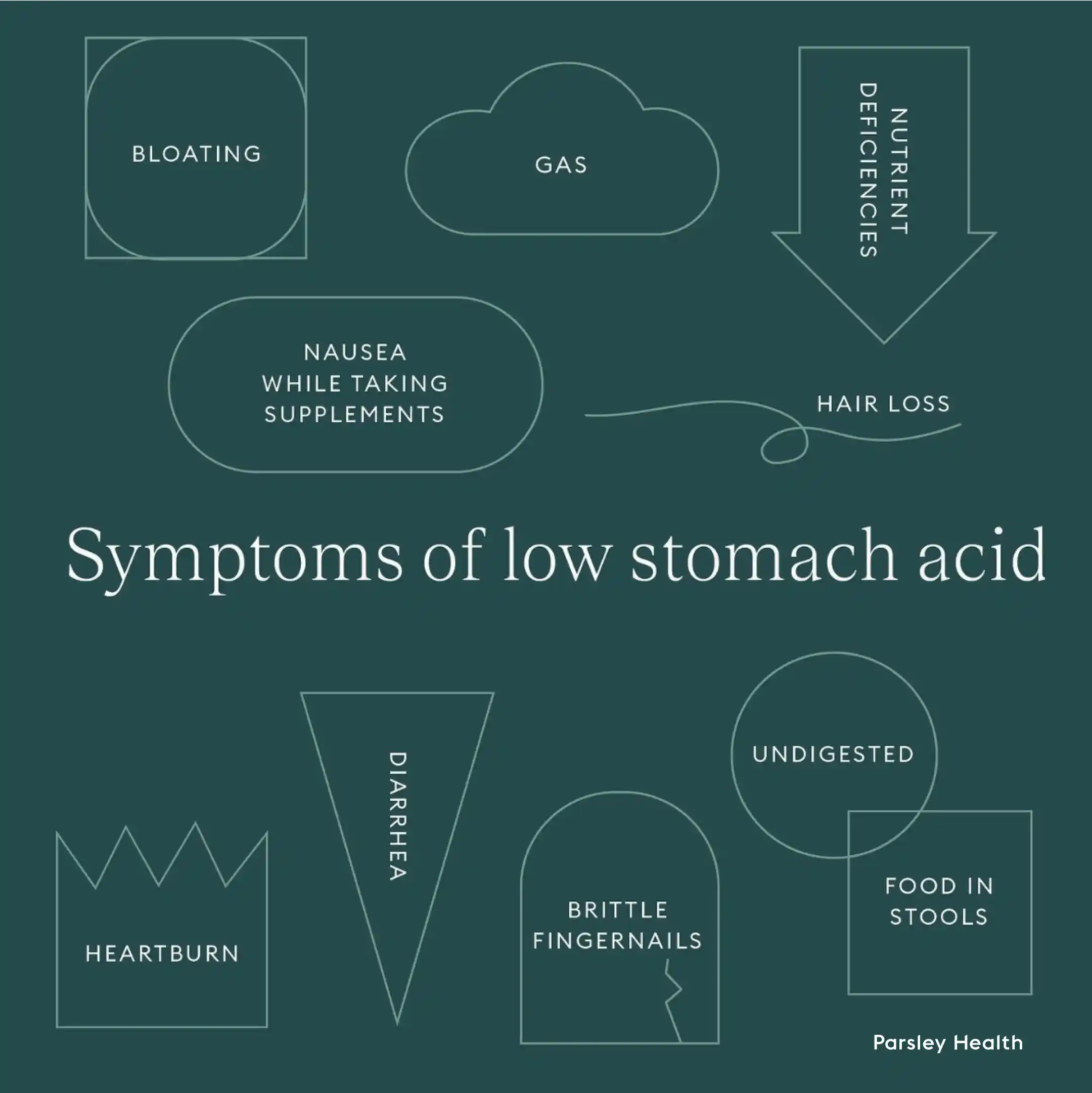
Some signs and symptoms of low stomach acid include the following.
bloating
undigested food in the stool
nausea while taking supplements
hair loss
brittle fingernails
Parsley Health providers often use a baking soda test, described here, to test stomach acid levels.
You’ve recently taken antibiotics
If you’ve been on a lot of conventional antibiotics like doxycycline recently—say, you were treated for Lyme disease—you may experience GI symptoms that could be fungal or bacteria related, or both.
“Just the way you can get a yeast infection after taking antibiotics, you can get fungal overgrowth in your gut, too,” Steinberg says.
If you do need to go on antibiotics, Steinberg recommends taking a probiotic containing the beneficial yeast Saccharomyces boulardii to help prevent SIFO.
Something’s slowing your gut motility
Anything that slows gut motility, the movement of food through your GI tract, is also a significant risk factor for SIFO and SIBO.
These include conditions like Type 2 diabetes and Ehlers-Danlos syndrome or if you’ve had a colectomy.
Sedentary behavior can also be a big one, says Steinberg, because it impairs blood flow to the digestive tract.
Anytime food sits in the small intestine longer, bacteria and fungi can take up residence and grow in numbers where they shouldn’t.
You have high alcohol consumption
Alcohol compromises the gut barrier and can fuel SIFO. Moderate alcohol use is also a risk factor for SIBO.
How is SIFO diagnosed?
Sometimes a clinical diagnosis is made if your GI symptoms fit the SIFO profile and you have other signs of fungal overgrowth, such as recurrent yeast infections.
Another sign of SIFO is if your symptoms worsen after consuming sugary, probiotic-rich, or vinegary foods and beverages.
But the “gold standard” for determining if someone has SIFO is with a duodenal aspirate (or a small bowel aspirate), says Dr. Steinberg.
This is performed during an upper endoscopy—a procedure in which a tubular instrument is passed through your esophagus and stomach and into a portion of the small intestines called the duodenum. From there, fluid can be collected and analyzed for the presence of abnormal fungi. This is also a way to test for SIBO.
Only a gastroenterologist can perform an upper endoscopy and duodenal aspirate. But, based on your results, doctors at Parsley Health can work in conjunction with your gastroenterologist to determine your best course of SIFO treatment.
How is SIFO treated?
SIFO treatment often requires a multipronged approach involving conventional or herbal antifungals and dietary and lifestyle changes.
Each individual’s specific SIFO treatment will depend on the severity of their case and their personal risk factors but may include the following.
Conventional or herbal antifungals
At Parsley Health, doctors often treat SIFO with conventional antifungal medications, such as fluconazole.
Natural antifungal and antimicrobial ingredients in herbs—such as olive leaf extract, grapefruit seed extract, and tea tree oil—may also be of benefit.
Do not ingest essential oils or extracts without the guidance of a doctor.
An anti-candida diet
Strategic dietary changes may also help limit fungal growth.
Cultured candida cells flourish when glucose is consumed, so scaling back on sugar and refined carbs may curb SIFO symptoms.
Steinberg advises some patients to temporarily eliminate refined carbs and sugars, most fruits, grains, and foods or drinks containing yeast. Items that contain yeast or yeast-like substances include the following.
alcohol
vinegar
pickled foods
sauerkraut
kefir
kombucha
You probably won’t need to eliminate these foods forever. Elimination diets are meant to be a short-term strategy to get your small bowel back to homeostasis, at which point you can eat a more balanced diet, explains Steinberg.
Movement and meal spacing
If low gastrointestinal motility is contributing to your SIFO, two big things can help improve it.
According to Steinberg, the number one way we can support healthy motility is through frequent movement throughout the day. She recommends taking regular walks (especially after meals), performing a few squat jumps and pushups, or doing anything that gets your blood flowing.
Additionally, space out your meals by three to five hours, and don’t eat within three hours of going to bed. Constantly having food in your stomach can impair one of your body’s key digestive mechanisms called the migrating motor complex.
The MMC is a recurring wave of movement that clears food out of the small bowel. It occurs every 90 minutes or so, but only when your stomach is empty.
Addressing low stomach acid
If your doctor or provider determines you have low stomach acid levels, they may recommend a hydrochloric acid (HCL) supplement.
HCL can help to bring stomach acid levels back to normal so you can adequately digest food, absorb nutrients, and kill off unwanted fungi and bacteria.
SIFO prevention and management
SIFO can return if you’re not addressing the underlying symptoms that contributed to it in the first place, like low stomach acid and low motility. While some dietary changes are meant just for the short-term treatment of SIFO, others are great for long-term prevention.
What to eat if you have SIFO
If you have SIFO or have been treated for it, you may wish to improve your diet in a sustainable way that also bolsters gut health.
Talk to your Parsley provider for a list of foods to add. What will be helpful for you may be different for someone else, based on your SIFO status, food sensitivities, or other gut health concerns.
Lifestyle management
Managing SIFO may involve a variety of lifestyle changes unique to your situation. For example, if you regularly need certain medications to manage an underlying condition, those medications could be impacting your gut health.
Talk to your doctor about your SIFO symptoms to see if certain medications are a culprit and if you can change those medications to another option.
Do not stop taking medications without talking to your doctor to see if doing so is safe.
Actions to take
If you suspect you have SIFO, you may be wondering about next steps. Here are some to consider.
When to see a health professional
You should talk to your doctor if you've developed unexplained GI symptoms. Your care team can investigate whether underlying conditions are causing abdominal discomfort.
Common questions to ask your doctor
You may have questions for your doctor at your appointment. Writing down your symptoms and a list of questions in advance will help you explain to your doctor what you've been experiencing and help you remember what you want to ask. Here are a few options.
Are any of my current medications causing my GI symptoms?
What tests can help investigate why I'm having GI symptoms?
Could my underlying conditions be causing my GI symptoms?
Should I change my diet, supplements, or anything else to help ease my GI symptoms?
What are our next steps in my care and treatment process?
Possible complications of SIFO
Left untreated, SIFO may lead to other GI issues. Some research indicates that SIFO has links to the following, but more research is needed to understand any potential mechanisms.
Crohn's disease
Gastric ulcers
Irritable bowel syndrome
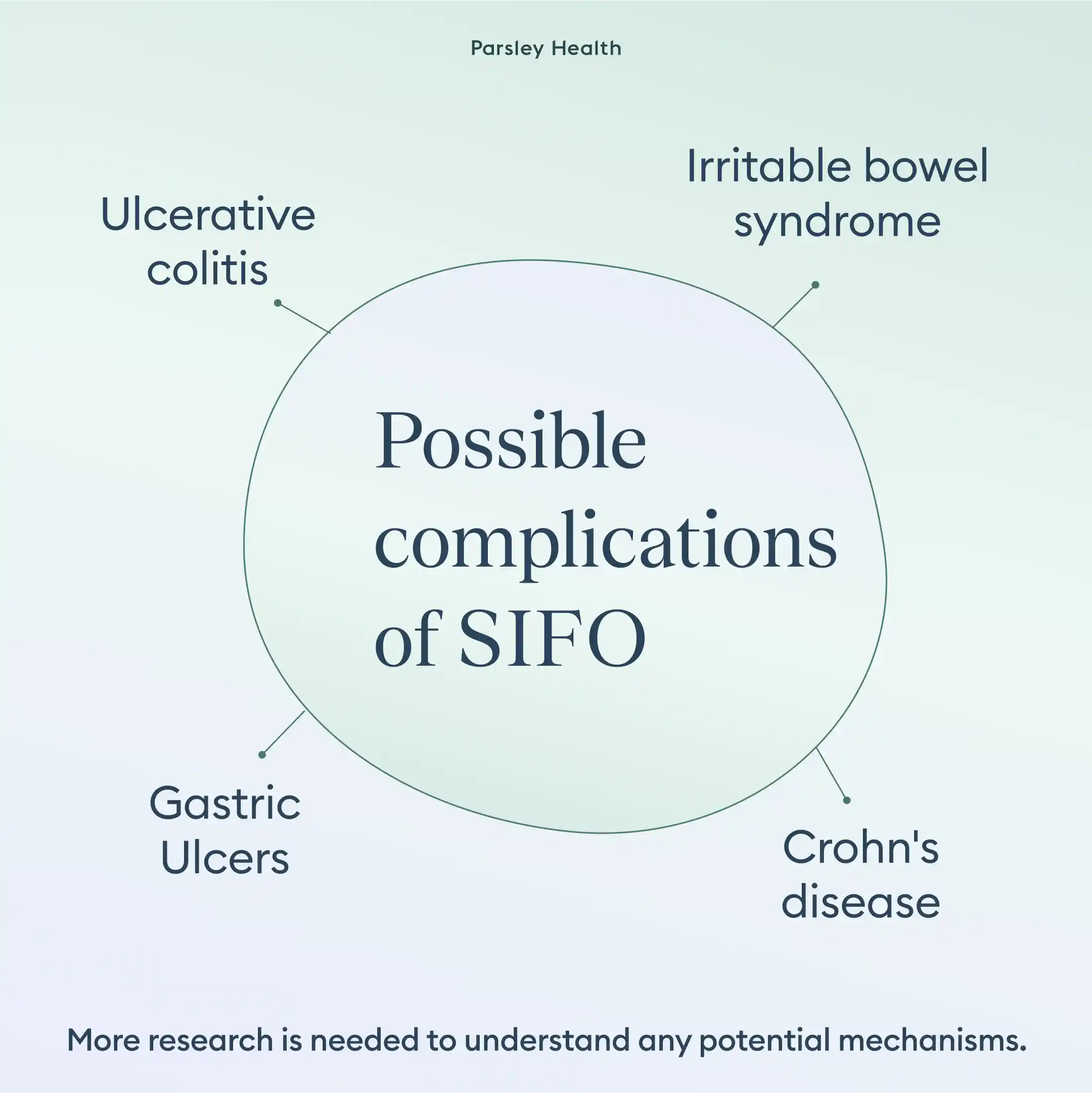
SIFO could also exacerbate your existing underlying conditions. So getting to the root cause of SIFO and treating it accordingly may help boost overall health.
FAQ
How do I know if I have SIFO?
Your doctor can diagnose SIFO by learning about your symptoms and conducting various tests.
How is SIFO diagnosed?
Your doctor can determine if you have SIFO by analyzing your symptoms and what exacerbates them and by conducting various tests. One of the best tests to diagnose SIFO is via a duodenal aspirate test, which involves an upper endoscopy.
What is the root cause of SIFO?
Several underlying factors can cause SIFO, including underlying conditions, a weakened immune system, low stomach acid, certain medications, and more.
What is the life expectancy of someone who has SIFO?
SIFO doesn't change your life expectancy.
What is the difference between SIBO and SIFO?
SIBO is when bacterial overgrowth occurs in the small intestine. SIFO is when fungal overgrowth occurs in the small intestine.
Bottom line
Treating and preventing SIFO requires a multifaceted approach. To make things more complicated, you could have SIFO and SIBO simultaneously, which will require a slightly different approach.
SIFO is tricky, which is why enlisting the help of a care team, like the doctors and other providers at Parsley Health, can be beneficial.
They can aid in diagnosis, come up with a tailored treatment plan, and provide the necessary long-term support that will keep your SIFO risk factors in check.

