This article has been medically reviewed by Nisha Chellam, MD.
You or someone you know have probably experienced a food intolerance or allergy; that’s how common they are. But for those who haven’t been able to pinpoint a specific food that’s causing their symptoms—or who have intermittent reactions to certain foods—there may be something else going on: histamine intolerance. Most people have never heard of it, but it’s more common than you might think.
What is histamine intolerance?
The term “histamine intolerance” might make it seem as if it’s a bad thing, but that’s not the case.
“Histamine is awesome,” says Sanna Kalika, MD, an internal medicine doctor at Parsley Health. It impacts immune function, helps get rid of infection, improves digestion, acts as a neurotransmitter and can improve cognition. In the right amount at the right time, it also improves blood circulation.
Histamine is a chemical made by the immune system that’s released from mast cells, a type of white blood cell. This happens in response to injury or allergen, and is the beginning of the inflammatory process, she explains.
If you come into contact with something you’re allergic to or intolerant of, histamine will act on many different parts of the body by: dilating blood vessels, causing your lungs to constrict, releasing adrenaline, spiking your heart rate, increasing capillary permeability, which causes swelling, and causing your skin to itch. In other words, it causes an allergic reaction.
“Histamine also triggers the release of stomach acid, so it helps us with digestion,” Dr. Kalika adds. But when histamine goes rogue, people experience symptoms of a histamine reaction on a regular basis. This is known as histamine intolerance.
What causes histamine intolerance?
One thing to get out of the way: You can’t actually be allergic to or intolerant of histamine. And it's not the same as having seasonal allergies or a food allergy, though it is similar.
“Histamine intolerance is simply having symptoms of too much histamine in the body,” Dr. Kalika clarifies. (So we call it a “histamine intolerance,” even though it’s technically not.)
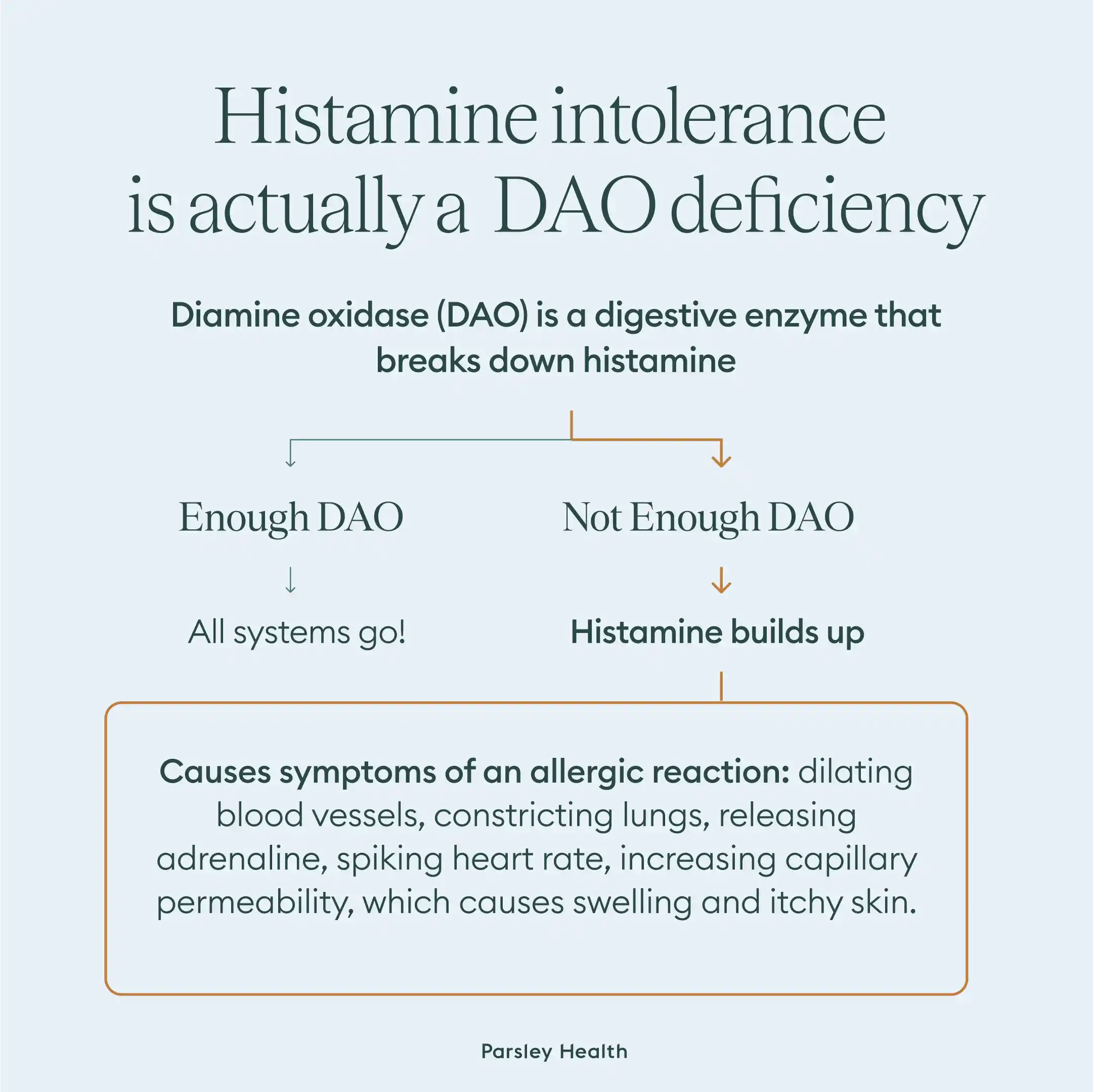
So why might that happen? We naturally produce a digestive enzyme called diamine oxidase (DAO) along with histamine that helps up break down the histamine we take in from food. (Almost all foods contain histamine, but some have much more than others.) DAO is produced by the kidneys, thymus, and intestinal lining.
But if we don’t have enough DAO, then we can’t break down histamine. “It can build up to high levels and cause symptoms, and these are the symptoms of histamine intolerance or overload,” Dr. Kalika notes.
According to Dr. Kalika, some common reasons for DAO deficiency include:
- Certain medications that block DAO production and/or function, such as NSAIDs and immune modulators
- GI issues like leaky gut, gut dysbiosis, IBD, SIBO, and other GI infections can affect histamine levels
- Eating too many histamine-rich foods, such as avocado, eggplant, and fermented foods—see full list below
- Genetics: genetic mutations can affect the production or activity of DAO and HNMT, leading to reduced histamine breakdown.
- Drinking alcohol
Histamine intolerance can also be caused by mast cell dysfunction, Dr. Kalika says, which can result in histamine overload. For example, an underlying cause can be mastocytosis, which is an increased number of mast cells, or mast cell activation syndrome, which is an increase in activation of existing mast cells.
It’s hard to say how many people are dealing with histamine intolerance, but a review in the American Journal of Clinical Nutrition estimated that 1% of the population has it, with 80% of them being middle-aged.
The symptoms of histamine intolerance vary widely.
Because histamine can trigger an inflammatory response in so many parts of the body, the symptoms can be incredibly vague.
The list of potential histamine intolerance symptoms is long, but some of the most common are related to the cardiovascular system, Dr. Kalika says. These include:
- Flushing, difficulty regulating body temperature, sudden excessive sweating
- Hives, rashes, swelling, itchy skin, eczema
- Racing heart, palpitations, arrhythmia
- Low blood pressure
But symptoms can also occur in the:
- Respiratory system, such as difficulty breathing, coughing (acute or chronic), asthma, nasal congestion, sinus issues, sore throat, post-nasal drip, and throat clearing
- Digestive system, such as nausea, vomiting, diarrhea, stomach pain, bloating, and acid reflux
- Nervous system, such as headaches, migraines, vertigo, dizziness, insomnia, fatigue, and anxiety
- Muscular system, such as muscle twitches, myalgia, arthralgia, and fibromyalgia
- Reproductive system, such as period cramps, irregular periods, endometriosis, and estrogen dominance
Histamine Intolerance Management and Treatment
Because the symptoms are so varied, histamine intolerance is usually diagnosed and treated by a process of elimination. There are no standardized tests to diagnose histamine intolerance. A histamine pinprick test may help suggest histamine intolerance, but it’s not a conclusive test.
Sometimes a doctor will prescribe a medication, such as an antihistamine. While this may stop symptoms in the short term, a 2020 study points out how medication doesn't get to the root of the problem.
That’s why diet is usually the first step in both diagnosis and treatment. In her experience over the years, Dr. Kalika says there’s one thing patients say that gives her a heads up they could be dealing with histamine intolerance:
“When people say they feel better when they eat worse, I suspect they have histamine intolerance. Because when they eat healthy, they may inadvertently consume a lot of histamine-rich foods.”
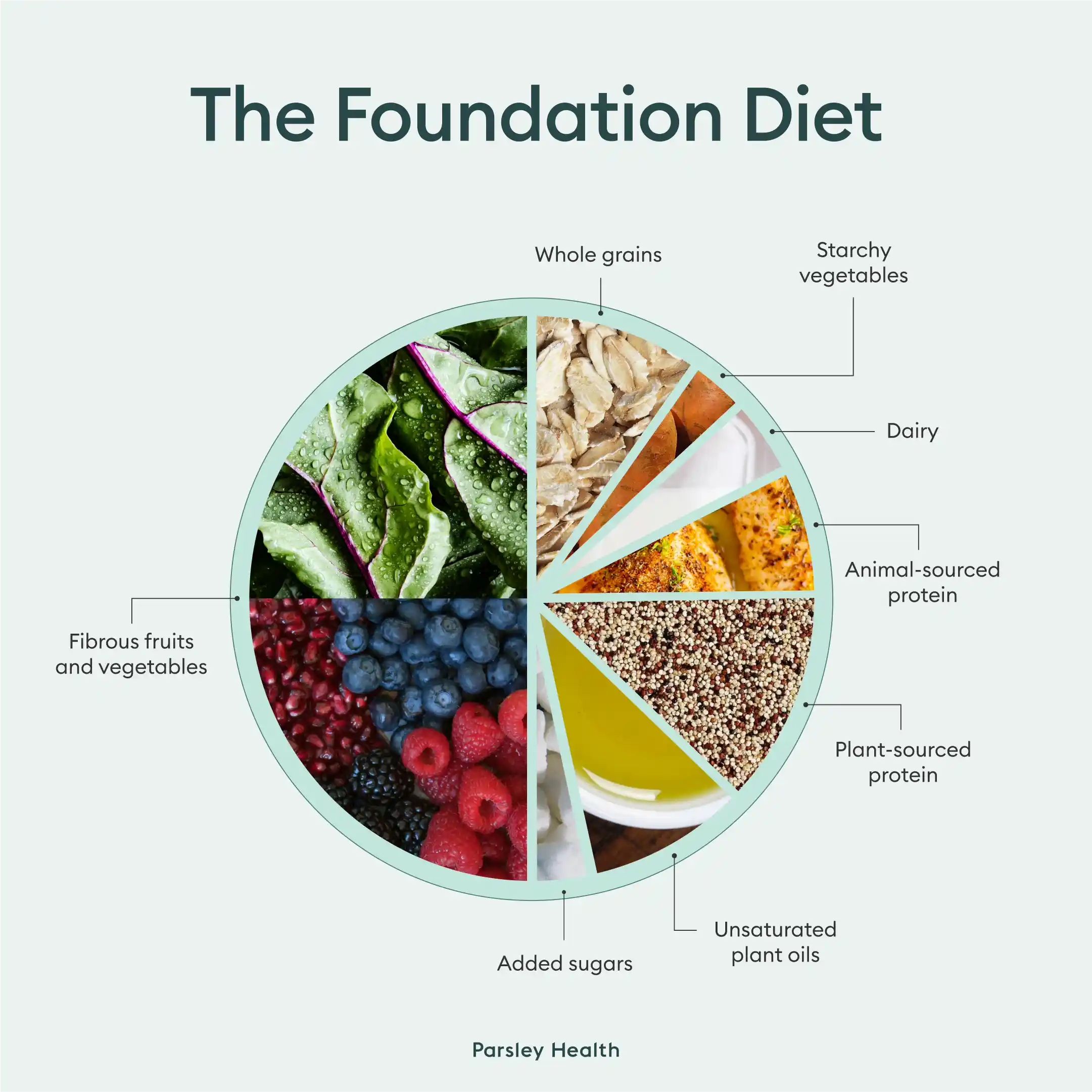
But before going directly to a low-histamine diet, Parsley practitioners recommend a foundational diet, Dr. Kalika says. This usually involves eating protein, greens, and healthy fats on every plate, while avoiding refined carbs, refined sugars, and trigger foods like gluten, dairy, and soy. “This is because if someone has symptoms of histamine intolerance due to an allergy to gluten or soy, a low-histamine diet will not get to the root cause.”
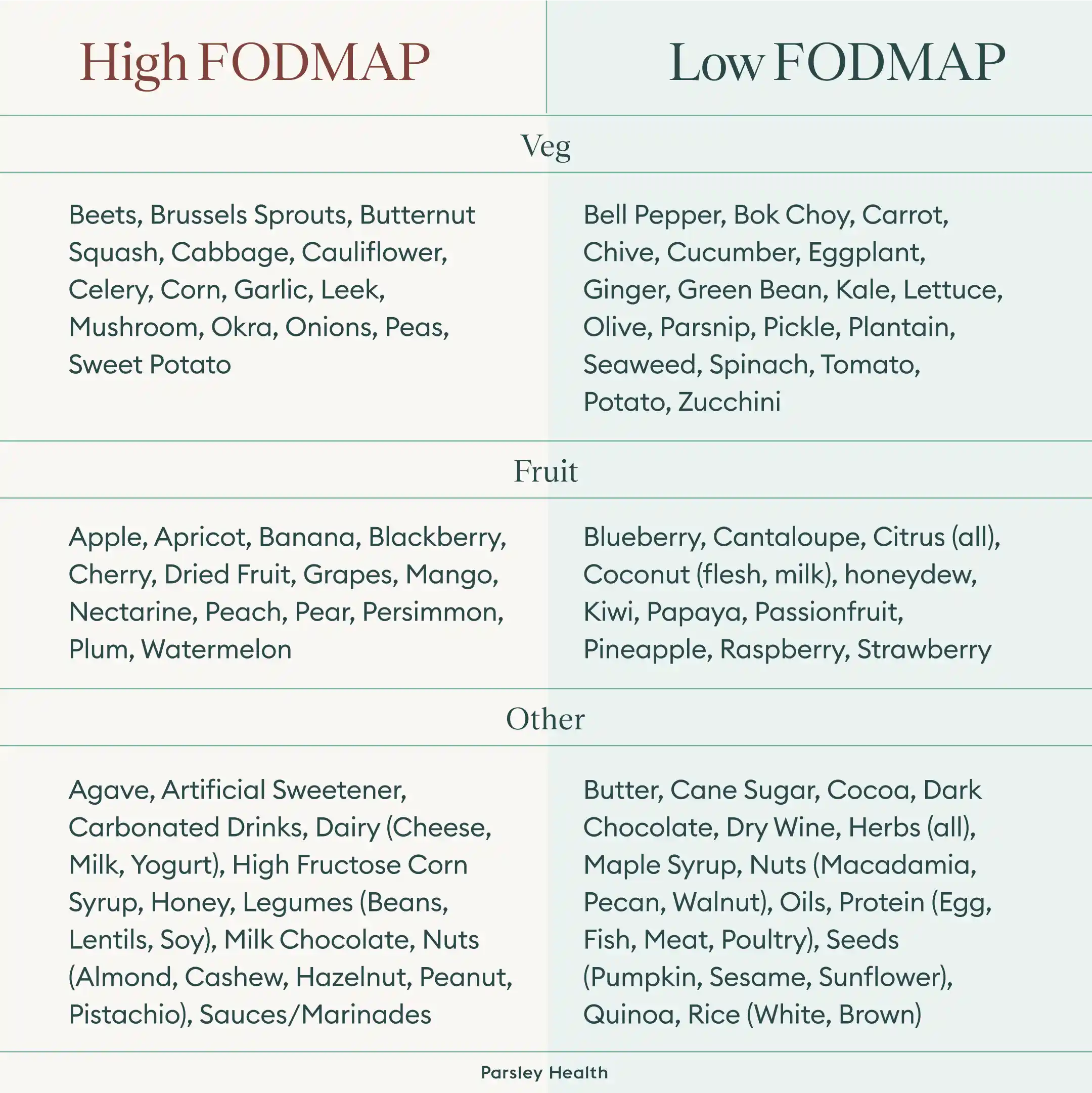
If that doesn’t work, next up is a low FODMAP diet. FODMAP stands for fermentable oligo-saccharides, di-saccharides, mono-saccharides, and polyols, which are types of fermentable carbohydrates some people have a hard time digesting. This can be because of a bacterial imbalance in their intestine, like SIBO, a sluggish digestive system that increases the transit time of food through the gut, or both. If a low FODMAP diet helps, that’s a sign that SIBO may be a factor, says Dr. Kalika. “If SIBO is diagnosed, the goal of the treatment is aimed at eradicating SIBO itself.” Once SIBO has been resolved, the histamine intolerance symptoms should, as well.
Only after trying both of these diets without symptoms resolving does Dr. Kalika recommend a low-histamine diet.
Plus, if you're looking to prevent a histamine intolerance, a 2021 study suggests the same diet used to treat it can prevent it as well. So whether you want to learn how to fix a histamine intolerance or prevent it, the following diet can help.
Histamine Intolerance Diet: Triggers to Avoid and Foods to Eat
Surprisingly, you don’t just avoid foods high in histamine. You also have to avoid foods that trigger histamine production and ones that block DAO production.
Foods that are high in histamines include:
- Fermented foods such as sauerkraut, soy sauce, and kimchi
- Vinegar and vinegar-containing foods such as pickles, mayo, olives
- Dairy products such as yogurt, kefir, sour cream and aged cheese
- Dried fruit
- Vegetables like avocados, eggplant, and spinach
- Processed or smoked meats and fish, like hot dogs
- Shellfish
Foods that trigger histamine release include:
- Alcohol
- Fruits like banana, papaya, and citrus
- Tomatoes
- Wheat germ
- Beans
- Chocolate
- Nuts, especially walnuts, cashews, and peanuts
- Food dyes and other additives
Foods that block DAO production include:
- Alcohol
- Black and green tea
- Energy drinks
A histamine-intolerance diet involves removing all the above foods. Then, each potential trigger food is reintroduced one at a time to watch for reactions. During this time, it’s important to focus on low-histamine foods such as:
- Fresh meat and fresh-caught fish
- Non-citrus fruits
- Eggs
- Gluten-free grains like quinoa and wild rice
- Dairy substitutes like coconut and almond milk
- Fresh vegetables, except for tomato, avocado, spinach, and eggplant
- Cooking oils like olive oil
“Diet-wise, some research also suggests that an adequate intake of healthy fats and other nutrients including phosphorus, zinc, magnesium, copper, iron and vitamin B12 may play a role in enhancing DAO activity,” Dr. Kalika says. So an overall balanced diet is key.
Sometimes, these dietary recommendations are also combined with other forms of treatment, including:
- Probiotics, since gut imbalance is a common cause of histamine intolerance
- Immunoglobulins, which boost the gut’s immune system, reducing histamine overproduction and improving DAO production
- Gut-soothing supplements like L-glutamine
- Traditional antihistamines
It’s also worth noting that some doctors may not know to look for histamine intolerance or may mistake intolerances for allergic reactions. According to Dr. Kalika, that’s because while there’s a lot of evidence in practice that histamine intolerance is an issue, there isn’t much published clinical research about it.
The good news? If you have a histamine intolerance, addressing the root cause should help resolve it over time, meaning you can enjoy histamine-rich foods again without symptoms. Finding that root cause can be a challenge, though, Kalika notes. “But at Parsley, we make an effort to identify the causes or triggers and work on eliminating them.”
Living with a Person With Histamine Intolerance
The best way to overcome a histamine intolerance is to change your diet. That means if you live with someone with this intolerance, your meals may look different too. By accepting these changes (and maybe even seeking out a few new recipes), you can help your loved one fix a histamine intolerance.
When to see a doctor
If unexplained symptoms pop up or you think you or a loved one has a food allergy, contact a healthcare provider. They can help you diagnose the underlying condition and create a treatment plan.
When at the doctors, it may be helpful to ask:
- Are these symptoms due to allergies or an intolerance?
- What in my diet might be causing this intolerance? How can I find my specific triggers?
- How can I adjust my diet to avoid symptoms?
The bottom line? Histamine intolerances are common and can be uncomfortable, but they are manageable. If you're concerned you have an intolerance, Parsley's physicians can help. Our team is skilled in diagnosing histamine intolerances and helping patients build a histamine intolerance diet.
Schedule a free call to learn more about Parsley’s virtual primary care, how to use insurance to pay for your Parsley medical fees, and more.
Frequently Asked Questions
How do you know if you are sensitive to histamine?
Figuring out if you're sensitive to histamine can be challenging, since it displays many symptoms similar to allergies. The most tell-tale signs are having a combination of intestinal symptoms, like bloating or constipation, and other symptoms, such as a stuffy nose, headaches, and eczema. The only way to know for sure, however, is a diagnosis from a healthcare provider.
How to fix histamine intolerance?
Fixing a histamine intolerance often comes down to adjusting your diet. A histamine intolerance diet often includes eggs, gluten-free grains, dairy substitutes, and fresh vegetables.
What do high histamine levels feel like?
High histamine levels can manifest in various ways. For some, high histamine feels similar to allergies, though these conditions are different. Others experience intestinal issues, like constipation, or skin problems, including eczema.
How to flush histamine out of your body?
A histamine intolerance occurs when there's too much histamine for our bodies to get rid of. Healthy individuals have enough of the enzyme intestinal diamine oxidase (DAO) to get rid of unwanted histamine naturally. If you have low DAO levels, you can "flush out" unwanted histamine through avoiding foods that block DAO production, such as alcohol and energy drinks.
