Progesterone as A Key Hormone for Women
Progesterone is a key hormone involved in the menstrual cycle, fertility, and pregnancy and it also plays a broader role in mood regulation, sleep, and overall hormonal balance. Levels naturally rise and fall throughout the menstrual cycle, particularly during the luteal phase. But for some people, progesterone levels may remain consistently low, which can contribute to a range of symptoms and health concerns. Some people may also need hormone replacement therapy.
Low progesterone is commonly discussed in the context of fertility and pregnancy, but its effects aren’t limited to reproductive health alone. People with low progesterone may notice changes in their cycle, heavier or irregular periods, mood shifts, anxiety, migraines, or difficulty sleeping. Understanding what influences progesterone production and when levels may be out of balance, is an important step toward addressing these symptoms thoughtfully.
So how do you increase progesterone, and when does it make sense to focus on supporting progesterone production? Can lifestyle changes help raise progesterone naturally, and when might medical options be considered?
In this article, we’ll explain what progesterone does in the body, common reasons progesterone levels may be low, and evidence-based ways clinicians support healthy progesterone levels—both naturally and, when appropriate, with medical care. As always, everyone’s hormone profile is different, and a personalized approach matters.
What is progesterone?
Progesterone is a key “female” hormone, but it’s important for the male body too. For people assigned female at birth, progesterone peaks in the luteal phase of the menstrual cycle, which begins after ovulation and ends when you get your period. During this time, your progesterone level looks a bit like a roller-coaster ride. It climbs to a steep height, starting around ovulation, and takes a plunge right before ol’ Aunt Flow arrives.
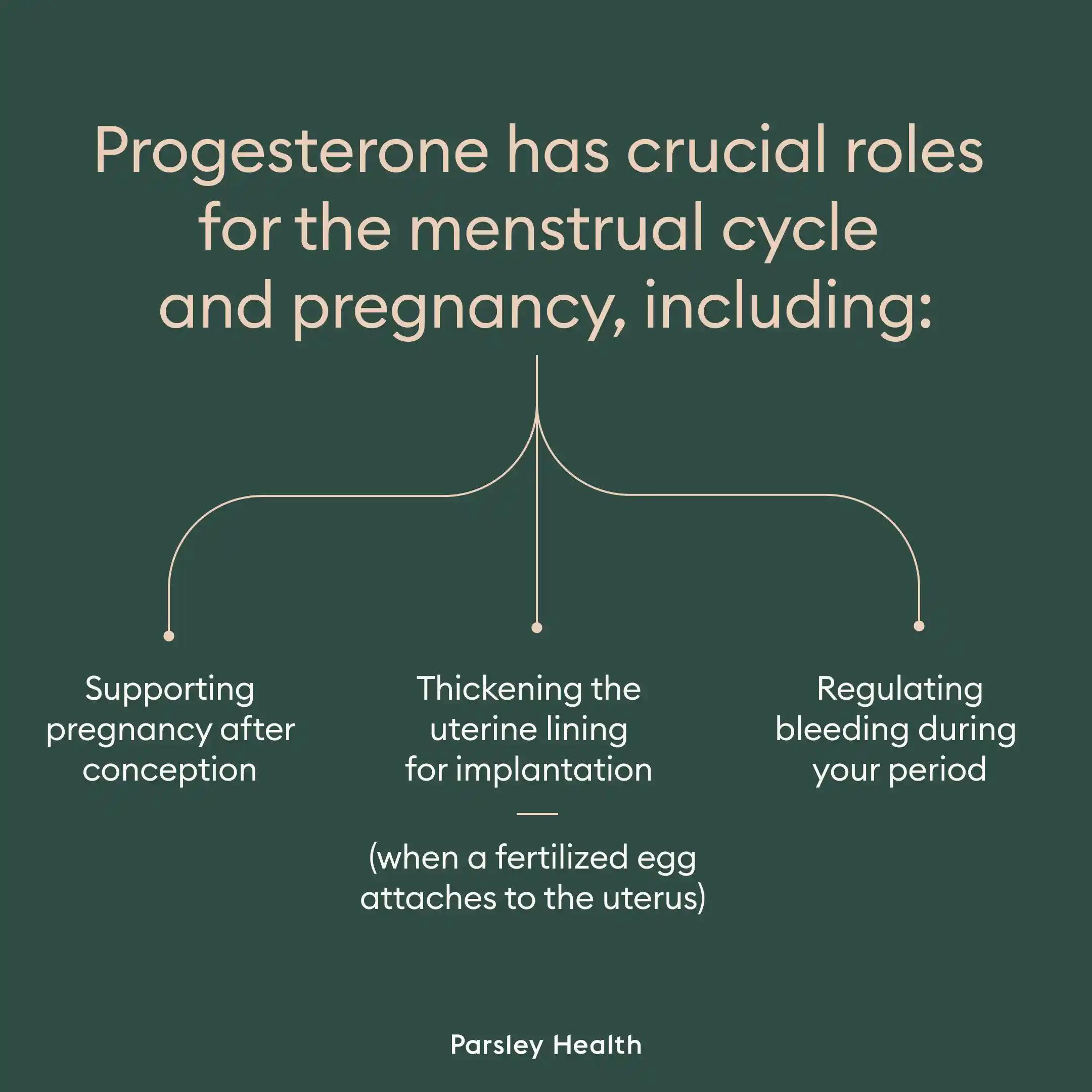
Progesterone has crucial roles for the menstrual cycle and pregnancy, including:
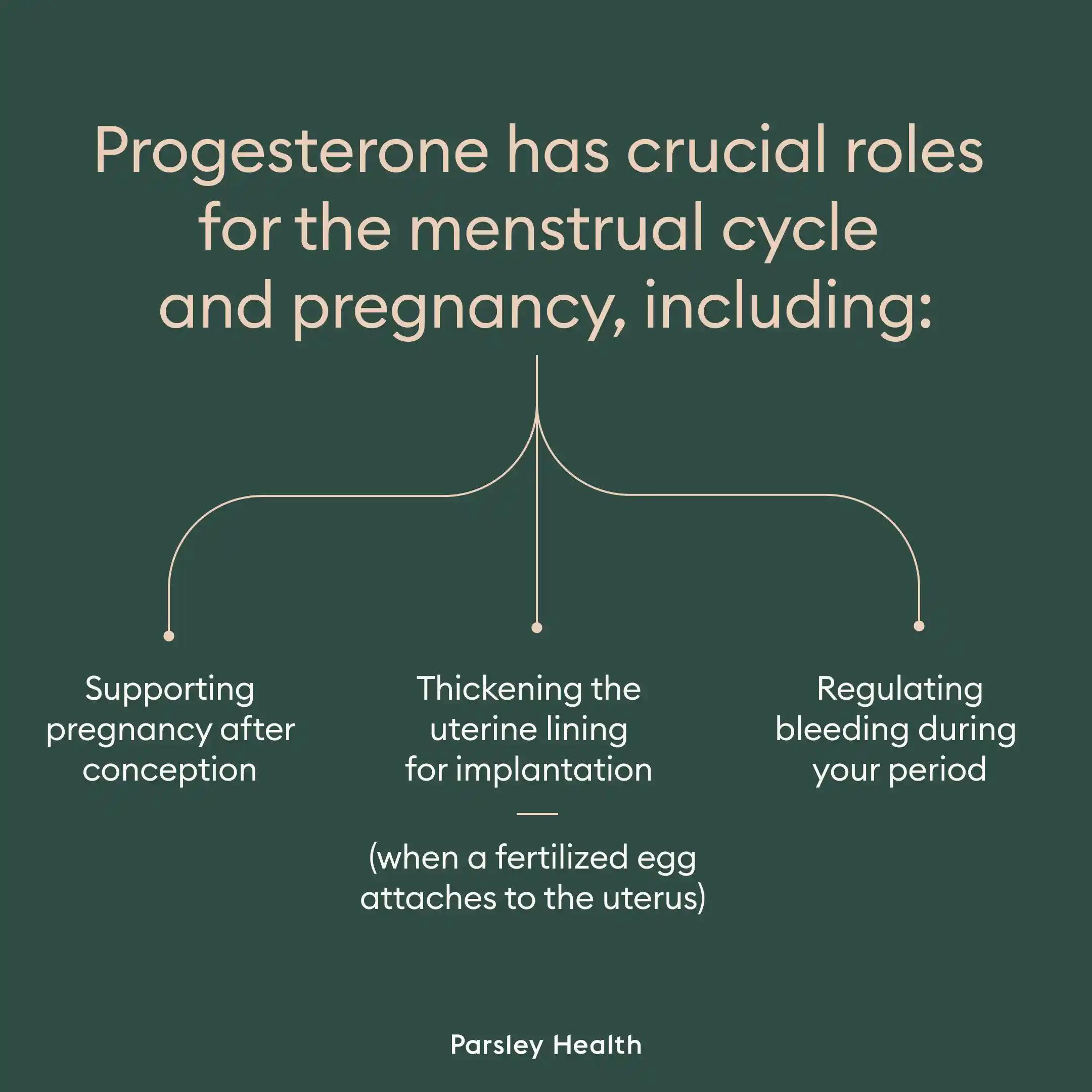
- Supporting pregnancy after conception
- Thickening the uterine lining for implantation (when a fertilized egg attaches to the uterus)
- Regulating bleeding during your period
Your progesterone level also impacts your mood and supports thyroid function.
Low progesterone is an issue for so many reasons, says Amy Beckley, PhD, a scientist who created Proov, an at-home FDA-cleared progesterone test kit. “It can make it harder to get and stay pregnant, as you need progesterone to support the uterine lining and hold a pregnancy,” she says.
Low progesterone or fast drop in your level can cause premenstrual syndrome (PMS) and its more severe form, premenstrual dysphoric disorder (PMDD), Dr. Beckley adds. And our brains have many progesterone receptors, so low progesterone can also cause mood swings and anxiety.
“It is the first hormone to drop during perimenopause and is what leads to those first symptoms of peri, like mood swings, trouble sleeping, hair loss, dry skin, weight gain, etc.,” Dr. Beckley says.
Symptoms of low progesterone levels
- Breast tenderness. Hormonal fluctuations can cause sore or tender breasts.
- Fatigue. Hormonal imbalances can affect your energy levels.
- Headaches or migraine. Hormonal changes associated with low progesterone can trigger headaches or migraine attacks in some individuals.
- Heavy or abnormal uterine bleeding. Estrogen dominance from low progesterone can lead to excessive growth of the uterine lining, resulting in heavy menstrual bleeding.
- Hot flashes and night sweats. These symptoms can arise, particularly during perimenopause when progesterone levels fluctuate.
- Irregular menstrual cycles. Low progesterone can cause irregular or absent periods, as it is essential for regulating the menstrual cycle.
- Low libido. Decreased sexual desire may occur as a result of hormonal imbalance.
- Menstrual cycle shortening. Cycles shorter than 24 days can indicate low progesterone levels.
- Mood changes. Symptoms such as anxiety, depression, and mood swings may occur as a result of the hormone’s influence on neurotransmitter function.
- Pregnancy complications. In pregnant people, low progesterone levels may lead to complications such as spotting, abdominal pain, and an increased risk of miscarriage.
- Spotting between periods. You may experience premenstrual spotting or bleeding if you do not have sufficient progesterone to stabilize the uterine lining.
- Vaginal dryness. Insufficient progesterone can contribute to dryness, affecting sexual health and comfort.
- Weight gain and fluid retention. Low progesterone can lead to increased fluid retention and weight gain due to its effects on metabolism and fluid regulation.
Factors that affect progesterone levels
What’s behind low progesterone? Several factors can lead to a lower level, from issues with ovulation to lifestyle factors, such as dealing with chronic stress, eating a low-quality diet, and engaging in either too much or not enough physical activity. (We need that Goldilocks’ just-right amount of exercise.)
Anovulation
If you aren’t ovulating (aka anovulation), you may have low progesterone. Ovulation causes an ovarian follicle to rupture and release an egg. The follicle then turns into the corpus luteum, a clump of cells on your ovary that releases progesterone, preparing the uterus for pregnancy.
Factors that can lead to anovulation
Estrogen dominance
Estrogen is another key “female” hormone, though it’s crucial for the male body too. Some issues can cause estrogen dominance, meaning the body has too much estrogen. This imbalance can lead to low progesterone.
Several conditions can cause estrogen dominance. I’m all too familiar with one of them: endometriosis (this is why I no longer have my uterus and left ovary). Endometriosis is a painful systemic inflammatory condition that causes endometrial-like tissue to grow outside the uterus. This tissue can then secrete estrogen. Other conditions associated with estrogen dominance include PCOS, uterine fibroids, and some types of breast and uterine cancers.
Environmental toxins
Icky things in our environment, specifically endocrine-disrupting chemicals, can also cause wonky changes to our hormones. “Microplastics, pollution, estrogens in the water and food supply all cause an imbalance in estrogen and progesterone, leading to lower progesterone levels,” Dr. Beckley says.
Stress
We all deal with stress now and then, whether you’ve got a work deadline staring you in the face or your furnace just died in the middle of winter and is costing you a fortune to replace. However, sometimes our stressors pile up faster than the laundry, leading to chronic stress.
When we’re stressed, our bodies produce cortisol, the stress hormone, to help us rise to the challenges we’re facing. But progesterone is an indirect precursor to cortisol, meaning that we can convert progesterone into the stress hormone, potentially causing low progesterone.
Too much exercise and a lack of adequate nutrition
Exercise has many bodily benefits, but overexercising can increase cortisol levels, which can then disrupt progesterone. This happened to me when I was once training for both an Olympic-distance triathlon and a marathon at the same time. Oops. During my aforementioned bout of overexercising, I was not supporting my body with enough nutrients. Double oops!
If you are engaging in extreme dieting or calorie restriction, you may not be able to support progesterone release. “You need a healthy diet to have the building blocks for progesterone,” Dr. Beckley says.
But even if you’re consuming enough calories, the quality proves just as important. Frequent glucose (blood sugar) spikes, from eating a diet high in refined carbohydrates and added sugar, can cause insulin resistance. Insulin resistance disrupts ovarian function and can lead to low progesterone.
Diagnosis and tests
Blood testing and salivary and urine tests can help determine your progesterone level. However, it will fluctuate throughout your menstrual cycle. So your clinician may wish to test you during a specific cycle phase or at multiple times.
How to Increase Progesterone Naturally
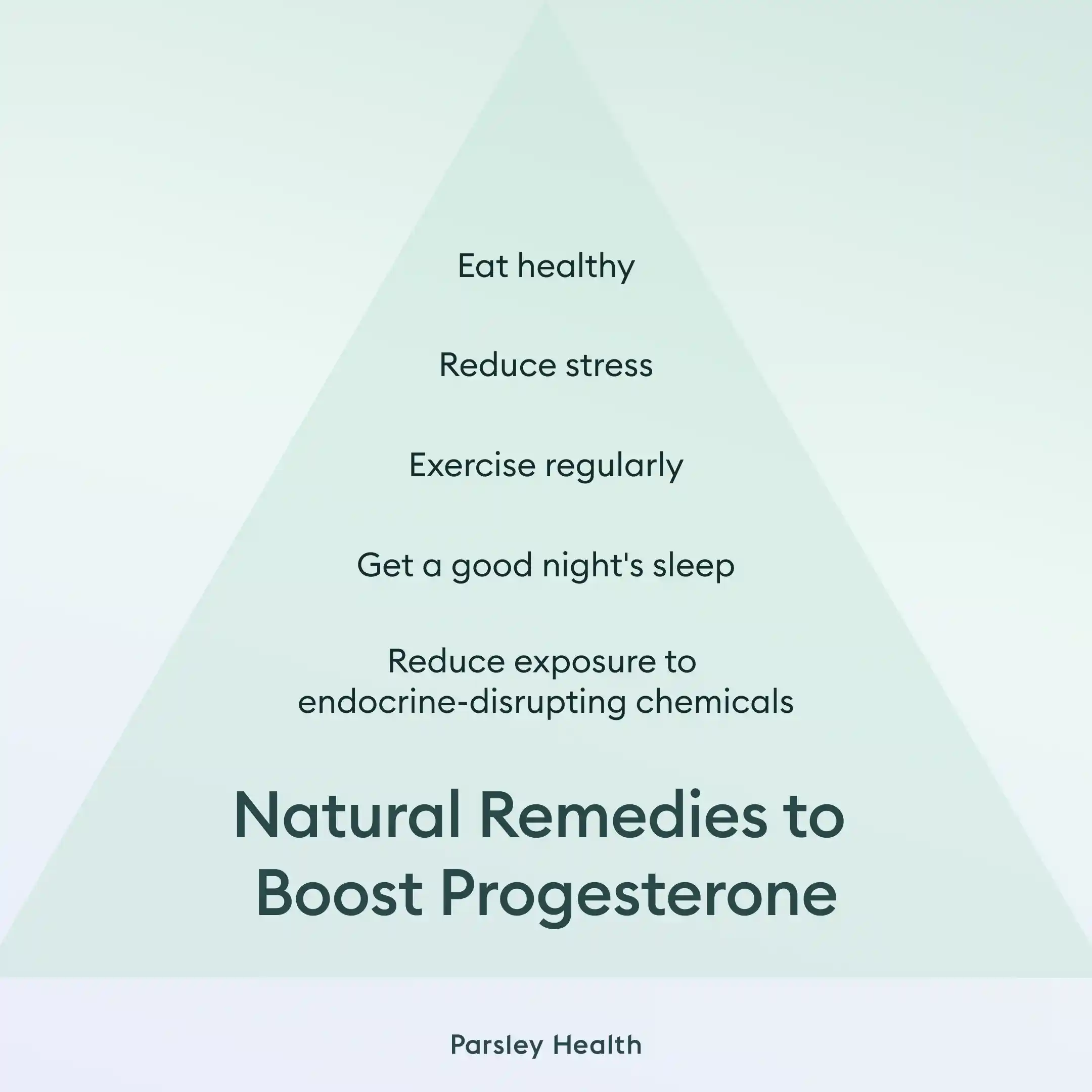
If you find out you have a low level, several lifestyle changes can help support progesterone production.
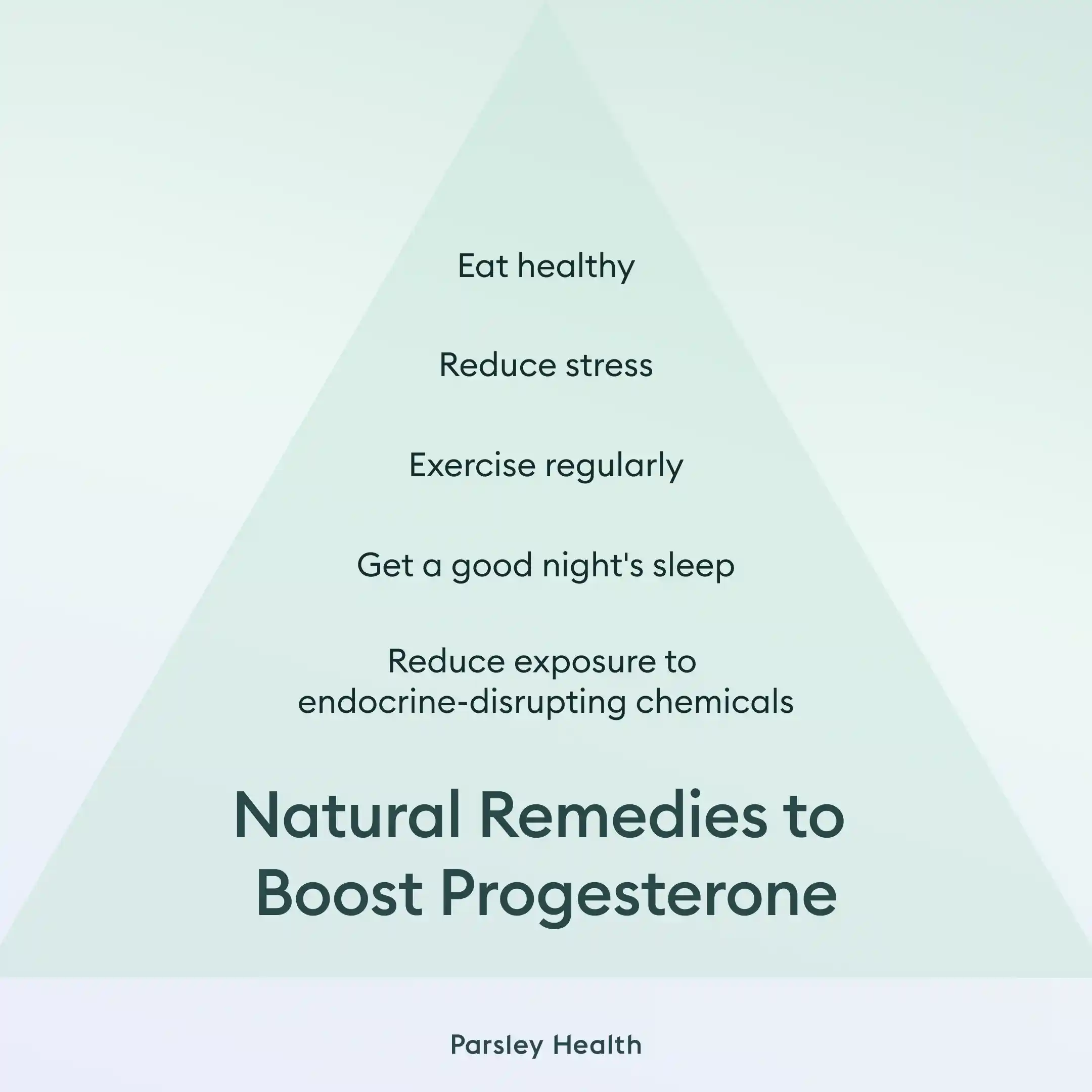
Eat a healthy diet
Stick to whole foods as much as possible, and eliminate ultra-processed foods, which often contain endocrine-disrupting chemicals as ingredients or in packaging. Reduce consumption of refined carbohydrates and added sugar, which can contribute to insulin resistance and disrupt ovarian function. You can also boost your certain vitamins and minerals intake to support your progesterone production.
Progesterone-supporting micronutrients
“There are also herbal supplements like red clover, Vitex, and Maca that can help you make more progesterone,” Dr. Beckley says.
Exercise regularly
Although overexercising can disrupt progesterone levels, exercise in general can be beneficial. Both cardio and strength training help, so try a mix of both. Exercise boosts insulin sensitivity, which can help support ovarian function. Likewise, exercise boosts HDL, a good type of cholesterol. Remember, our bodies make progesterone from cholesterol, so the good kind is what you want to elevate.
A note of caution: You may find that your energy level decreases when you’re in the luteal phase, aka the week or so leading up to your period. This is completely natural and happens to many of us, including me. I’ll be on a run during this phase and I’ll find I can’t sustain the pace I could the previous week. I’ve learned now that my body needs me to back off during this time.
In the luteal phase, your body is directing energy resources to your uterus for reproduction, so aim for lighter activities during this week. You may also feel fatigued on the first few days of your bleed and prefer to stick to low-key styles, such as restorative yoga or walking.
Get good sleep
Lots of things can disrupt your sleep, from your mind running amok the minute you hit the pillow (guilty!) to a snoring partner. But good quality and quantity sleep are crucial for hormonal support. A lack of sleep can make you more insulin resistant the next day. Over time, this can lead to disrupted ovulation. Sleep loss can also elevate cortisol, which can then lower progesterone. Aim for at least seven hours, but you may need even more.
Invest in an eye mask and ear plugs if light and noise pollution plague you, and ditch screens at least 30 minutes (though more is better) before bed. Also, create consistent sleep and wake times to support your body’s natural clock, which also regulates hormones.
Reduce stress
Remember, high cortisol can potentially interfere with progesterone. If you’ve been running on a steady diet of stress, find ways to alleviate it. Eating a healthy diet, getting adequate physical activity, and focusing on quality sleep are all great ways to start. But you might also consider yoga, meditation, a favorite hobby, or anything else that gives you a dose of calm.
Reduce exposure to endocrine-disrupting chemicals
Unless you can find a way to live in a completely healthy bubble (if you do, let me know!), you can’t fully eliminate exposure to endocrine-disrupting chemicals. But you can decrease how much of these nasties you’re exposed to. When buying personal care products, household cleaning products, furniture, and other items, check if they’ve got the green light from the Environmental Working Group.
Non-natural methods to boost progesterone
“Medically, you can simply take bio-identical (or body-identical) progesterone,” Dr. Beckley says. “This can be in the form of a pill, injection, cream, oil, and vaginal suppository.” A knowledgeable clinician can test your hormone levels and then prescribe one of these products if needed.
Risks and considerations
Progesterone supplementation may have side effects. That’s why working with a clinician is best.
Common side effects of progesterone supplements include
- Abdominal cramps
- Back pain
- Breast tenderness
- Dizziness
- Vaginal bleeding
More severe effects can include
- Low blood pressure
- Blood clotting
You may not be a candidate for certain types of hormone replacement therapy if you’ve had a blood clot, stroke, heart attack, or breast or endometrial cancer, or if you have active liver disease or unexplained vaginal bleeding. Working with a knowledgeable clinician can help you determine what’s safest and best for you.
Frequently Asked Questions About Increasing Low Progesterone Levels
How can I increase my progesterone levels quickly?
Increasing your progesterone level will take time and won’t happen overnight. This article explores ways to naturally and medically support your hormone levels.
Can you fix low progesterone?
Yes, you can fix low progesterone through lifestyle changes, though in some cases you may need hormone replacement therapy.
How do I know if I have low progesterone?
You can ask your clinician for a simple blood test to determine if you have low progesterone.
How much B6 is needed to increase progesterone?
The amount of B6 your body needs to support progesterone will depend on your age and your pregnancy or breastfeeding status. Adults 19 to 50 years old should ensure they are getting 1.3 milligrams of B6. If you are assigned female at birth and over 51, aim for 1.5 milligrams. If you are pregnant, you will need 1.9 milligrams, and if you are breastfeeding, you will need 2.0 milligrams.