Hives and rashes are often used interchangeably, but they’re not the same thing. While hives are a specific type of rash, not all rashes are hives, and understanding the difference can make it easier to identify what’s happening on your skin and how to address it.
The term rash refers broadly to any change in the skin’s color, texture, or appearance. Rashes can look red, scaly, bumpy, inflamed, or irritated and may be caused by a wide range of factors, including allergies, infections, irritants, or chronic skin conditions. Hives (also called urticaria), on the other hand, are a distinct type of rash characterized by raised, itchy welts that often appear suddenly, move around the body, and typically fade within 24 hours.
“Hives are a distinct type of rash characterized by raised, itchy welts that can appear suddenly, shift location, and usually fade within a day,” says Srdjan Prodanovich, MD, FAAD, a board-certified dermatologist. “In contrast, ‘rash’ is a broader term that includes many different skin reactions, such as eczema, contact dermatitis, or infection-related inflammation.”
Because symptoms can overlap, itching, redness, swelling, it’s easy to confuse hives with other types of rashes. Factors like how long the skin reaction lasts, whether it changes location, and what seems to trigger it can offer important clues.
Below, we’ll walk through a clear head-to-head comparison of hives vs rash, including what they look like, common causes, and how treatment approaches may differ.
Hives vs Rash: What Are The Differences?
Both hives and other types of rashes result from your immune system reacting to a trigger and releasing chemicals that cause inflammation to help protect the body.
To understand the difference between hives and rashes, we need to unpack what they are. First, as Dr. Prodanovich notes, hives are also considered a rash. But they’re just one type of a rash, which is more of an umbrella term.
“’Rash’ is a broad term that covers inflammation of the skin, including hives, psoriasis, eczema, bumps, and more,” says Melanie Palm, MD, MBA, a board-certified dermatologist at Art of Skin MD. “Hives are a type of rash that are often characterized by red or skin-colored welts. They often feel intensely itchy and sometimes come with a burning or stinging sensation.”
- Rashes occur when an area of skin features a change in texture, color, or appearance; a rash is also called a “sudden skin eruption.” Causes vary, from bacterial or fungal infections, allergic reactions, inflammation and irritation, autoimmune disorders, and more.
- Hives, a type of rash, are also called urticaria; hives are wheals or welts, which are raised areas of the skin. They occur because mast cells have released histamine and other chemicals related to the immune system. Hives usually itch, but not always.
Not sure what your symptoms are really telling you?
The Parsley Symptom Index helps connect the dots across your whole body so you can understand patterns, not just isolated symptoms.
Hives vs Rash: Do They Look Different?
Again, hives are a type of rash, but they often look distinct from other rashes because they appear as wheals or welts due to swelling on the surface of the skin. The welts may match your skin color or look blotchy. They can be small, like the size of an erasure on the end of a pencil, or they may be much larger, such as the diameter of a pint glass or even a salad bowl. Their edges can also blend together. They are sometimes circular or more elongated or irregularly shaped.
 Rashes are much more complicated to describe because each type of rash varies in appearance, and the same type of rash can look different from one person to the next. A rash might present with a change in hue compared to your usual skin color. A rash may be red, pink, purple, gray, silver, white, or just darker in general. A rash also often features a change in texture, such as bumps, spots, cracks, or scales. However, a rash can also be a smooth but inflamed patch of skin.
Rashes are much more complicated to describe because each type of rash varies in appearance, and the same type of rash can look different from one person to the next. A rash might present with a change in hue compared to your usual skin color. A rash may be red, pink, purple, gray, silver, white, or just darker in general. A rash also often features a change in texture, such as bumps, spots, cracks, or scales. However, a rash can also be a smooth but inflamed patch of skin.
How do you know if your rash is hives or if it’s a different type of rash? Imagine you’ve spilled water on a sealed hardwood floor or wooden deck. It beads in irregular shapes on the surface. Hives match this general beading appearance. However, how long your rash lasts and your specific symptoms can offer some additional clues.
Location and duration
Hives and rashes can appear on any part of the body. So location isn’t always a helpful way to distinguish whether you have hives or another type of rash. However, some autoimmune rashes show up in specific locations. For example, a rash related to systemic lupus erythematosus typically appears across the nose and bridge of the cheeks.
Duration can be a bit more helpful. Unless you have chronic urticaria, which lasts or goes away and reappears, the one-off bout of hives tends to go away within 24 hours. Other rashes, however, can last for days, weeks, or even longer, depending on the cause.
Hives also tend to have a sudden onset, meaning they develop quickly, whereas other types of rashes can either appear quickly or gradually over time.
Symptoms to help you tell the difference between rashes and hives
Your symptoms can also offer some clues.
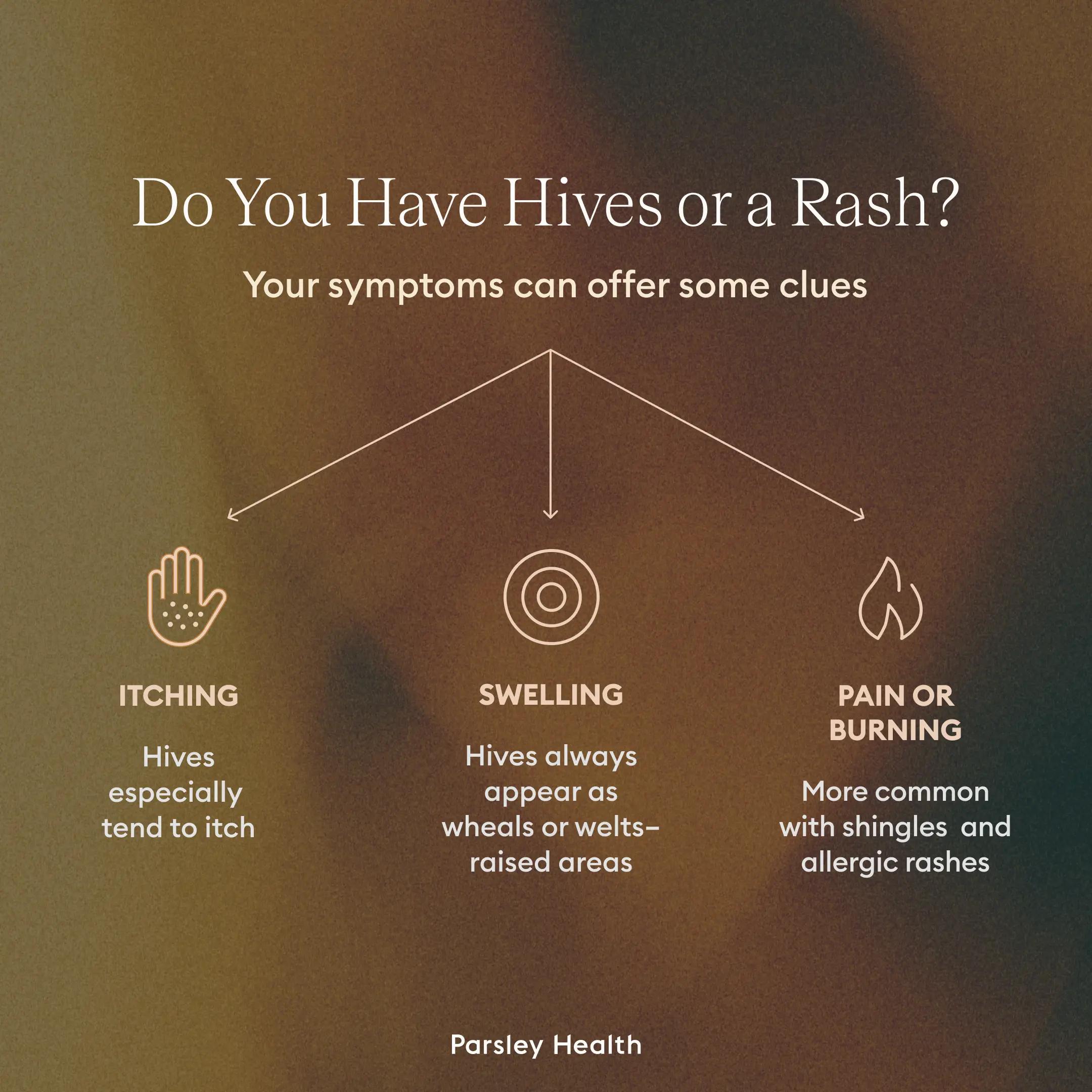 Itching. Hives especially, but also other types of rashes, tend to itch, though this is not always a characteristic.
Itching. Hives especially, but also other types of rashes, tend to itch, though this is not always a characteristic.- Swelling. Hives feature swelling because of blood vessels leaking fluid into the surrounding tissue. Other types of rashes sometimes cause swelling, as well, but again hives always appear as wheals or welts–raised areas.
- Pain or burning. Hives and other types of rashes can also burn; however, these symptoms are more common and severe with shingles rashes and contact dermatitis, an allergic rash.
Healing stories from our members
Common causes of hives and rashes
Any conversation about triggers for rashes and hives should come with an explanation about the term “idiopathic” Sometimes this word, which means the cause is unknown, gets tacked onto the word urticaria, such as in the phrase “chronic idiopathic urticaria.”
That doesn’t mean that the hives are in your head. Obviously, you can see them on your skin. It just means the cause isn’t clear. A knowledgeable and caring provider will not dismiss your symptoms, however. Instead, they will work to get to the root cause.
“In many chronic cases, called chronic idiopathic urticaria,” Dr. Prodanovich says, “no apparent external cause is identified. However, research shows that a significant number of these ‘idiopathic’ cases are linked to autoimmune thyroid disease.”
Other forms of autoimmunity may also be a culprit. Up to 45 percent of chronic urticaria cases have associations with autoimmunity. This was true for my hives, originally deemed chronic idiopathic urticaria. Subsequent testing eventually revealed my MCAS diagnosis, which has links to autoimmunity.
Common triggers for hives
“Hives occur when an allergic reaction triggers the release of histamine into the skin, causing an inflammatory response,” Dr. Palm says.
Common allergy triggers
- Foods (e.g., tree nuts, eggs, shellfish)
- Insect bites or stings
- Pet dander
- Medications (e.g., antibiotics or non-steroidal anti-inflammatory drugs, aka NSAIDs)
- Environmental factors (e.g., bare skin on grass)
Chronic activation of mast cells, causing hives, can also occur from Type 2 helper T (Th2) immune dominance, meaning the immune system is overactive, which leads to an increase in immunoglobulin E (IgE) antibodies that drive allergic reactions. This dominance may occur from exposure to environmental toxins, gut dysbiosis, and more.
And histamine intolerance occurs when the body can’t break down histamine properly, which can lead to a hives eruption.
“Other factors like autoimmune conditions, stress, physical stimuli (for example, sudden temperature changes or exposure to extreme hot or cold), and even sunlight can trigger hives in some people,” Dr. Palm says.
“Stress doesn’t typically cause hives,” Dr. Prodanovich adds, “but it can intensify or prolong them. Emotional or physical stress triggers the release of histamine, which fuels itching and inflammation, and cortisol, which, when chronically elevated, may dysregulate immune function and weaken the skin barrier. I frequently see patients with chronic urticaria experience flare-ups during stressful life events, underlining the connection between psychological stress and skin conditions.”
A subset of hives is called dermatographia. This type appears as a result of pressure, scratching, or rubbing. For example, if a cat scratches me, or even if I scratch myself, I will develop a hive in the shape of the scratch. Just by scratching me, you can literally “write on my skin” which is what the term “dermatographia” means.
Common triggers for rashes
Listing triggers for other types of rashes gets a bit more complicated since they vary depending on the type of rash.
- Allergic reactions
- Autoimmune conditions or autoimmunity (e.g. psoriasis, psoriatic arthritis, etc.)
- Friction (e.g., from clothing)
- Heat (miliaria, a “heat rash” caused by blocked sweat glands)
- Infections
- Injury
- Irritants
- Viruses
Signs you should see a doctor
“You should seek medical attention if hives or rashes last more than a few days, recur frequently, or are accompanied by facial or throat swelling, difficulty breathing, fever, or severe pain,” Dr. Prodanovich says. “These symptoms may indicate a life-threatening allergic reaction (anaphylaxis) and require immediate emergency care.”
Parsley Health offers physician-led functional medicine care, advanced lab programs, and flexible ways to get started, all designed to help you feel better over time.
Diagnosis and testing
After you talk to a knowledgeable care team, your clinician may ask you questions about your symptoms, examine your affected skin, and ask you about your medical history.
Some testing may be required to determine if you have allergies and, if so, what you are allergic to. In other cases, your provider may request laboratory tests to look at allergic or immune-system markers.
Treatment options for hives and rashes
Your treatment options for hives or another type of rash will depend on the underlying cause. For example, a rash from an infection may require antibiotics or antifungal medications, which may be oral, topical, or both.
If you have an autoimmune disorder that’s causing your skin issues, then your provider will work with you to manage the underlying condition. Treatments may include lifestyle changes, medications, and more.
For short-term relief, you have a few options. “Antihistamines, which are available over the counter, are typically the first line of defense for treating hives,” Dr. Palm says. You can take these orally or apply a topical cream.
Over-the-counter (OTC) hydrocortisone creams are also an option for hives and other types of rashes. However, you should check with a provider first to ensure you’re using an OTC product that’s right for you.
If you know what triggers your rash or hives, avoiding the trigger can be helpful. However, that’s not always possible. For example, I mentioned my odd trigger of going from cold to warm environments. I typically can’t avoid this in winter without simply staying inside all the time. (No thank you!) However, if your hives result from a food allergy or an allergy to a specific detergent or fabric, then avoiding the trigger will reduce the chance of hives recurring.
A functional medicine approach to managing hives and rashes
Functional medicine offers a multilayered approach to treating rashes and hives by addressing the various triggers identified through testing. This integrated treatment strategy typically includes:
- Personalized dietary interventions, including elimination diets and anti-inflammatory nutrition plans
- Gut-healing protocols to restore intestinal barrier function and balance the microbiome
- Targeted supplementation to address nutritional deficiencies and support immune function
- Strategies to address environmental triggers and toxin exposure
- Stress-management and mind-body techniques to address psychological triggers
- Lifestyle modifications, including sleep optimization and exercise recommendations
Natural and holistic relief approaches
Some natural options for relieving the itching, burning, or irritation associated with hives or rashes include the following.
- Cool it down. A cold compress, or cool shower or bath can help reduce hive-related swelling and the inflammation that drives itching or irritation of most rashes.
- Take an oatmeal bath. Add a colloidal oatmeal product to your bath, or grind the oatmeal in your pantry into a powder and add it to your soak. Oatmeal combats inflammation and relieves itching and irritation.
- Reduce stress. If stress is a trigger for your hives or another type of rash, engage in stress management techniques regularly.
- Consider your nutrition. An anti-inflammatory diet may be of benefit to help keep skin conditions in check, especially those related to autoimmune conditions or autoimmunity.
Key takeaways
- Hives are just one type of rash, but many other rashes can also appear on your skin.
- Hives are distinct because they appear as raised welts; other types of rashes have a different appearance, depending on the cause.
- Working with a knowledgeable care team, such as the folks at Parsley Health can help you get to the root cause of any skin changes. Reach out for a free consultation.
Frequently asked questions about hives vs rashes
How to tell if it’s a rash or hives?
Hives are a type of rash. You can tell if you have hives based on how your skin looks. Hives appear as raised wheals or welts and look a bit like water beading on a sealed hardwood floor or deck. Other types of rashes will look different from each other and different from hives.
What triggers hives?
Allergic reactions, autoimmune conditions, stress, and more are all triggers for hives.
Should you take Benadryl for hives?
Benadryl (diphenhydramine) is an over-the-counter antihistamine used to treat hives and other allergic reactions. However, if you are older or have any underlying conditions or take medications, you should consult your healthcare provider before using Benadryl.
How do you confirm hives?
To confirm whether your skin changes are hives or another type of rash, you should consult a knowledgeable clinician.
How to cure hives fast?
Antihistamines, either oral or topical, are first-line treatment for hives. However, cold compresses and colloidal oatmeal baths are other options that will help soothe your skin.



 Rashes are much more complicated to describe because each type of rash varies in appearance, and the same type of rash can look different from one person to the next. A rash might present with a change in hue compared to your usual skin color. A rash may be red, pink, purple, gray, silver, white, or just darker in general. A rash also often features a change in texture, such as bumps, spots, cracks, or scales. However, a rash can also be a smooth but inflamed patch of skin.
Rashes are much more complicated to describe because each type of rash varies in appearance, and the same type of rash can look different from one person to the next. A rash might present with a change in hue compared to your usual skin color. A rash may be red, pink, purple, gray, silver, white, or just darker in general. A rash also often features a change in texture, such as bumps, spots, cracks, or scales. However, a rash can also be a smooth but inflamed patch of skin.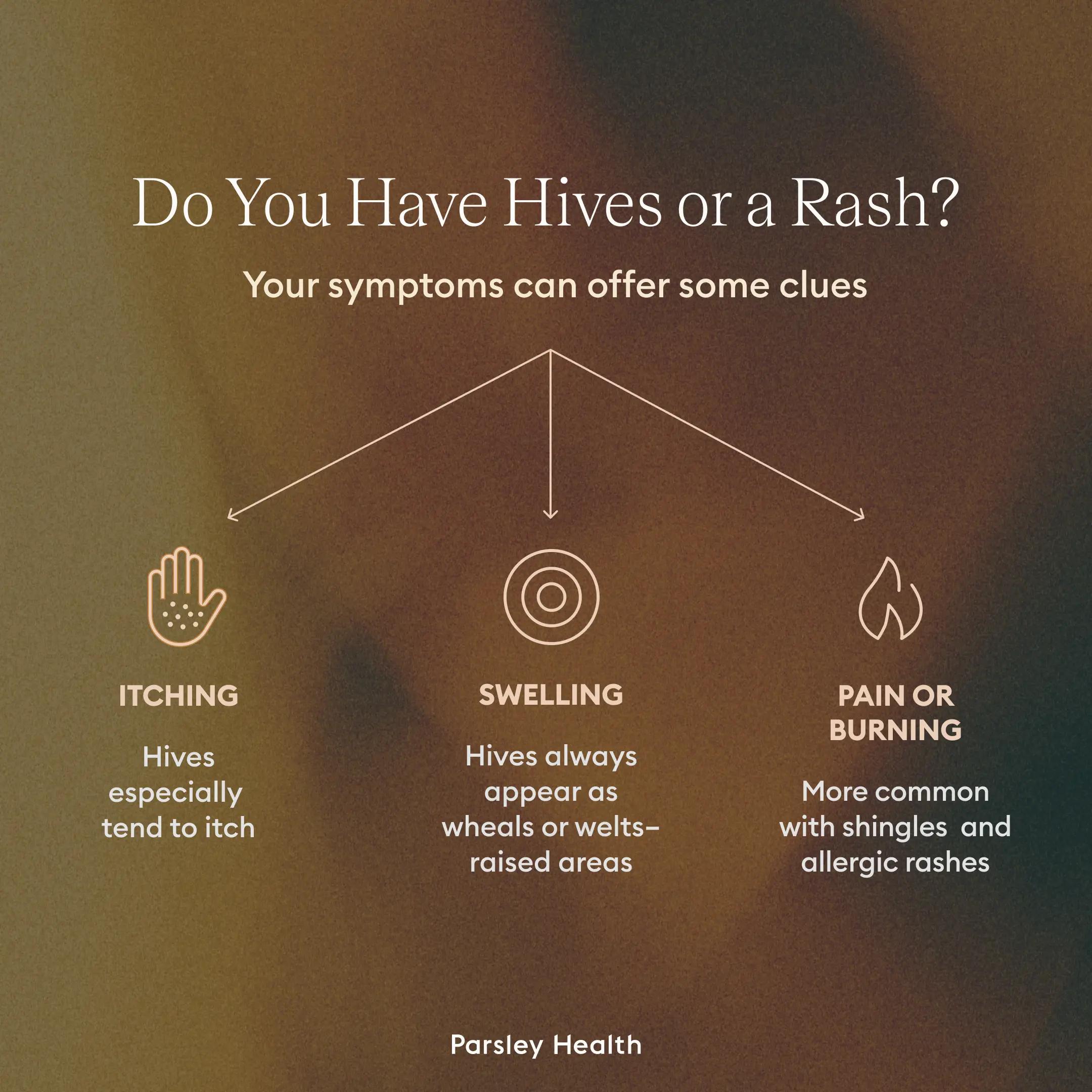 Itching. Hives especially, but also other types of rashes, tend to itch, though this is not always a characteristic.
Itching. Hives especially, but also other types of rashes, tend to itch, though this is not always a characteristic.



