Sleep is elusive for so many of us. But what does it mean when you’re still tired after eight hours of sleep? Good sleep isn’t just measured by how many hours you get; sleep quality matters, too. Sleep timing, daytime habits and bedtime behaviors, stress and anxiety, sleep interruptions, and health conditions can all make sleep less refreshing. Tackling sleep struggles requires a whole-body approach. Looking at ways to improve your health, sleep hygiene, nutrition, and mental well-being can all combine for a better night of rest.
Our hope after sleep is to wake up feeling alert and refreshed. To make it through a day without excessive caffeine chugging or the desire to snooze in a meeting. Unfortunately, that’s not the reality for many of us. If you’re asking yourself why do I wake up tired after eight hours of sleep? you’re not the only one. Sleep problems are rampant, and more than one in three U.S. adults get insufficient sleep each night, according to the Centers for Disease Control and Prevention (CDC).
So many things factor into good rest. Daytime habits, before-bed behaviors, stress, nutrition, and underlying health problems all influence how well you snooze. Uncovering what’s at play for you individually can take time and effort—and some medical expertise, too. Here’s what you need to know about why you’re feeling tired after sleeping, plus the steps you can take to improve your sleep.
How sleep works
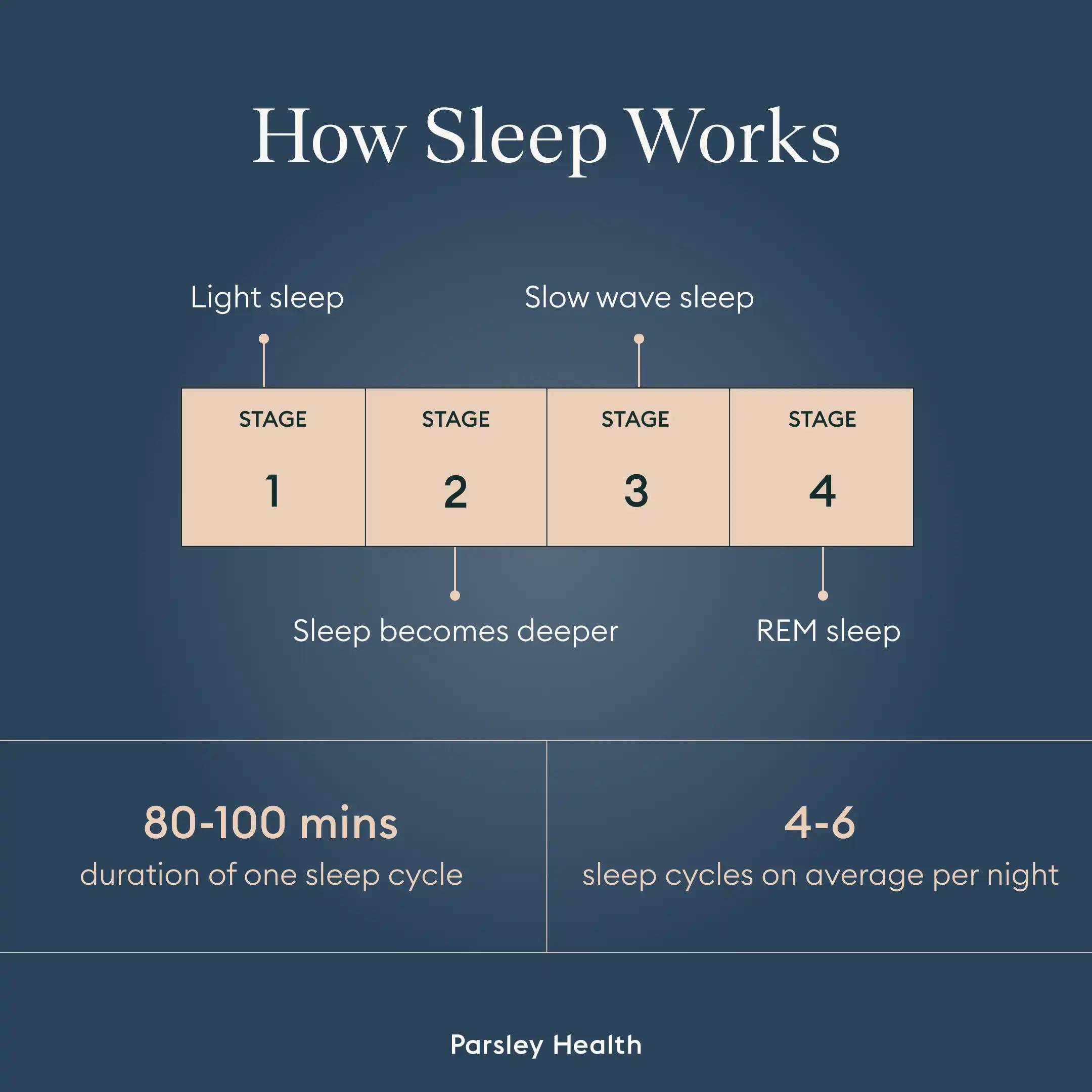
After you fall asleep, you move through several sleep cycles per night. One cycle consists of both non-REM and REM sleep.
Non-REM sleep
REM stands for “rapid eye movement.” There are three stages of Non-REM sleep:
Stage 1: Light sleep. This is the transition between being awake and sleeping.
Stage 2: Deeper sleep. This stage aids in functions like memory consolidation.
Stage 3: Deepest sleep. It’s also referred to as slow-wave sleep. It’s tough to wake people up from this stage. Tissue repair and growth occur here. If you wake up during this stage, you’ll have “sleep inertia,” that feeling of total where-am-I-right-now? grogginess that can take up to an hour to shake off.
REM sleep
During REM sleep, your brain is highly active and you dream. Luckily, muscles in your arms and legs are temporarily paralyzed so you don’t act those dreams out! (Critical muscles, like those that control your respiratory system, remain functional.)
Together, one cycle of non-REM and REM sleep lasts 80 to 100 minutes. You go through about four to six of these sleep cycles per night.
Common reasons you wake up tired after 8 hours of sleep
Just because you’re in bed for eight hours doesn’t mean you’ve had good sleep. Sleep quality is key in how refreshed you feel in the morning. It’s based on several factors that all combine into how good your sleep is, says Jade Wu, PhD, board-certified behavioral sleep medicine psychologist and founder of Thrive Behavioral Sleep Medicine Clinic. These factors include:
Sleep duration.
Consistent timing of sleep.
Sleep habits that are in alignment with your natural chronotype (one’s biological tendency to be a “night owl” or “early bird")
Restfulness of sleep, which includes getting enough of each stage of sleep
Sleep consolidation (few interruptions)
If you’re waking up tired after eight hours of sleep, it’s a good idea to consider the environmental factors and lifestyle habits that are interrupting your sleep, says Wu. Maybe:
Your sleep environment is too hot or cold, too noisy, or has too much light (such as outdoor lights or lights on electronics in the room).
Your sleep partner is snoring.
Your pets sleep with you in bed and they’re loud or move around too much.
You’re getting too much light at night and/or too little during the day. Light exposure regulates your circadian rhythm (or body clock).
You have too much stimulation during the evening.
You go to bed or wake up at inconsistent times of the evening.
You consume caffeine or alcohol too close to bedtime and/or in excess.
Finally, certain diseases and undiagnosed sleep disorders can lead to fewer hours of sleep, poor quality sleep, less restorative sleep, and lower daytime energy, including:
Chronic pain conditions like fibromyalgia
Asthma
Gastroesophageal reflux (acid reflux and heartburn)
Chronic kidney disease
Viral illnesses
Lyme disease
Cancer
Sleep apnea
Restless legs syndrome
Narcolepsy
REM sleep behavior disorder
The above is certainly not an exhaustive list, and it’s something to talk to a functional medicine provider about. These are medical professionals who are keyed into how critical sleep is for your overall well-being. They regularly talk to patients about how their health status affects their sleep and, conversely, how their sleep affects disease management.
Stress and sleep
Stress (which we all experience because, hey, we’re human) can contribute to insomnia and decrease sleep quality. “Stress can make sleep more difficult, as it can keep the body or mind more tense or activated,” says Wu. Even being stressed out about sleeping or not getting “good enough” sleep can cause sleep disruptions. Unfortunately, lack of sleep also makes these problems worse.
After a poor night of sleep, you may feel groggy, low on energy, and under brain fog. You didn’t need research to tell you that—but there are many studies that show that sleep loss is a drag on your mood and negatively affects your ability to emotionally regulate. (As someone who has burst into tears in the grocery store after a horrible night of sleep, I can relate.)
More alarming than the short-term effects are the long-term impacts of your sleep habits. Sleeping both too little or too much is associated with depression, found research on U.S. adults in the Journal of Affective Disorders. Lack of sleep is also associated with symptoms of anxiety, too.
If it’s stress or anxiety standing in the way of your sleep, there are certain things you can do to help your brain “turn off” before bed, says Wu:
Journal, which allows you to do a brain dump of things that are on your mind. “The idea is that once you’ve gotten this out of your system a bit, your mind is less likely to worry about these topics when you go to bed,” Wu says.
Practice gentle yoga or try a mindfulness meditation.
Go to bed sleepy, not just tired. The idea being that you don’t want to give your mind the time and space to worry, or associate bedtime with the opportunity to start swirling worries around in your head.
Use distraction to get your brain off the worry track. Wu recommends an audiobook or podcast, but make sure whatever you’re listening to is interesting but not stimulating. (Think a topic that relates to your hobbies, not a crime podcast.)
If sleep loss is negatively impacting your mood and emotions, the most important piece of the puzzle is to address underlying sleep problems. That includes medical problems or hormonal changes. Lifestyle habits like poor sleep hygiene or stress can also factor in. Many times, there is a combination of these to address.
Impact of diet and nutrition on sleep quality
When it comes to how well you sleep, what you eat (or don’t) matters. Although more studies are needed, research in Sleep Medicine Reviews suggests that “healthier” diets are related to better sleep quality compared to diets containing more processed foods and sources of added sugar. These healthier diets contained high intakes of:
Fruits
Vegetables
Whole grains
Legumes (beans, peas, lentils)
Olive oil
Seafood
The foods above provide nutrients that support good sleep and regulate your circadian rhythm. Antioxidant-packed foods may also help reduce inflammation, which can have a negative impact on sleep.
Finally, there’s some evidence that inadequate intake of certain nutrients is associated with poor sleep (less than seven hours per night), found in a study in Nutrients:
Calcium
Magnesium
Vitamin A
Vitamin C
Vitamin D
Vitamin E
Vitamin K
Some people will benefit from supplementing with certain nutrients to optimize their intake of these vitamins and minerals. Talk to a functional medicine provider about tests to analyze your nutrient status. You can then work together to make a plan to fill in the gaps via diet changes and possible supplements.
Exercise and physical activity for better sleep
One of the best things you can do for your sleep is move on a daily. One research review in Cureus has found that physical activity is linked to better sleep quality and less time it takes to fall asleep. For people who struggle with insomnia, exercising can be part of your treatment plan.
So what’s behind the power of breaking a sweat? Exercise releases feel-good chemicals like endorphins and neurotransmitters that quash stress and anxiety to promote relaxation. The official recommendation is to clock 150 minutes of moderate-intensity activity (brisk walking, light jogging) per week, along with twice weekly strength training. You can break this up into smaller bouts (like 10 minutes) if it fits better into your schedule.
One thing to consider is how the timing of exercise and type of workouts affect how well you sleep that night. Some people will find that a high-intensity workout right before bed is too activating, making it hard to doze off. Others may not be bothered at all. Reviewing how you react may help decide to move your HIIT to morning or stick to a post-work cycling class.
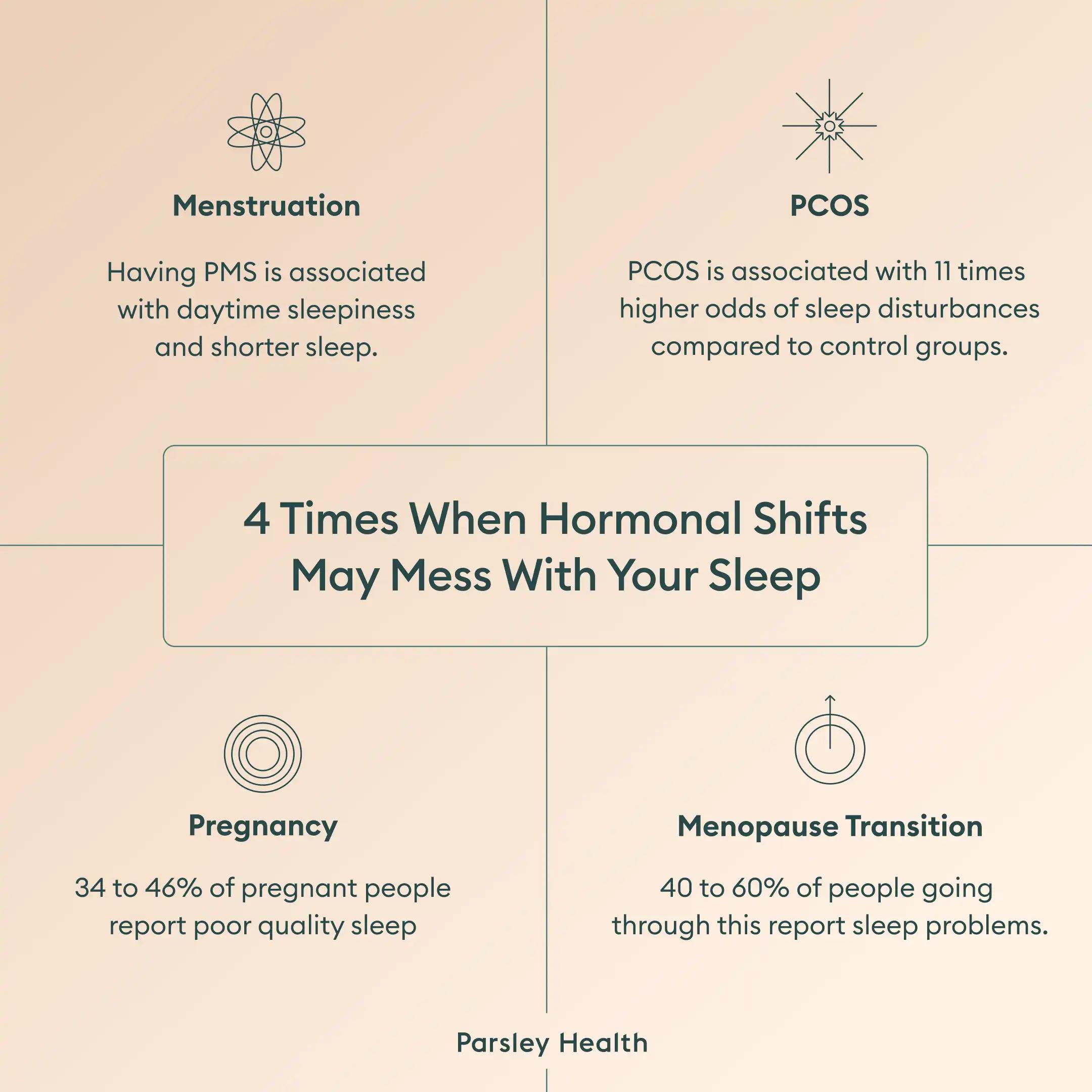
Hormonal changes and sleep
Hormone changes can affect your sleep in various ways, such as by causing symptoms (like night sweats) that disturb your sleep. They’re also associated with an increased risk of sleep disorders (such as sleep apnea or restless legs syndrome). Here are three times when hormonal shifts may mess with your sleep:
With menstruation, having PMS or dysmenorrhea (painful periods) is associated with poor sleep, daytime sleepiness, difficulty falling or staying asleep, and shorter sleep.
Having PCOS is associated with 11 times higher odds of sleep disturbances compared to control groups, according to one review.
During pregnancy, 34 to 46% of women report poor quality sleep.
Within the menopause transition, 40 to 60 percent of midlife women report sleep problems.
Addressing hormonal changes requires a comprehensive hormonal screening to assess hormonal balance and a whole-body approach in treatment that incorporates lifestyle factors (like sleep hygiene, below), exercise and healthy nutrition, managing stress, supplementation, and more.
Sleep hygiene and lifestyle tips
Sleep hygiene is the things you do to promote good sleep. They can occur during the day (such as waking up at the same time each day, exercising, or going outside for light exposure), as well as the things you do right before bed to transition to sleep.
When it comes to your before-bed habits, create an enjoyable bedtime routine. This will help you wind down before sleep, says Funke Afolabi-Brown, MD, a sleep medicine physician and founder of RestfulSleepMD. This is good for relaxing your body and mind, both of which will ease you into sleep. “Maintaining a consistent routine is important. Make sure your sleep environment is ideal, avoid device use before bed, and don’t consume caffeine, alcohol, or heavy meals before bed,” Dr. Brown recommends.
The best bedtime routine will look different from one person to the next, and it doesn’t have to be particularly long or complex. “If you’re having sleep problems, look at the root cause–are there specific habits you have that do not support good sleep? That’s a great place to start,” she says.
“The brief overarching recommendation I give is to treat sleep like a friend–make time and space for it, prioritize the relationship with it, but don’t be so overbearing that you add stress to the whole situation,” adds Wu. Trying too hard to have ‘perfect’ sleep can backfire, so you’re better off honing in on a few things that will move the needle on your sleep quality.
Here are four habits Wu recommends focusing on as a start:
Be consistent in the time you get up in the morning.
Go outdoors for at least 30 minutes per day.
Be physically active every day.
Protect your sleep environment from disruptions.
It’s also a boon to connect with a professional (see below) for more tailored advice based on your specific underlying sleep challenges. Addressing those will make the biggest difference in bettering your sleep for the long haul.
Signs that indicate a sleep problem
Sleep isn’t always easy and quick. There may be the occasional day when it’s hard to fall asleep or you want to doze off during a meeting. But there are certain signs that you may have a sleep disorder, and it’s worth getting checked out by a clinician. Here are some of them:
You need more than 30 minutes to fall asleep.
You have frequent night wake-ups or wake up too early in the morning.
You feel sleepy during the day or fall asleep during the day (when not intending to nap).
You snore, gasp, make choking sounds, or stop breathing during the night. (This may indicate sleep apnea.)
You have symptoms of restless legs syndrome, including creeping, tingling, and crawling feelings in your arms and legs.
You have symptoms of narcolepsy, including cataplexy (sudden muscle weakness during strong emotions).
If you’re struggling with sleep, keeping a sleep diary can help you track your sleep patterns. This can also be done using an app or a sleep-tracking device. If your clinician is concerned that you may have a sleep disorder, they may recommend seeing a sleep specialist. A sleep study may be recommended to diagnose a sleep disorder if one is suspected.
When to seek professional help
If you’re experiencing persistent fatigue despite feeling as if you’re getting eight hours of sleep (or being in bed for eight hours), consult with a functional medicine provider. In certain cases, you may also be referred to a sleep specialist or advised to have a sleep study performed. If you have insomnia, then consulting a behavioral sleep medicine specialist, psychologist, or therapist who can provide cognitive behavioral therapy for insomnia (CBT-I) can help you revise your habits, behaviors, and thoughts around sleep to improve your sleep quality and duration.
Finally, pursuing an integrative approach to sleep problems will give you a well-rounded look at your sleep, since there may be several factors preventing you from getting good rest, including nutrition gaps, caffeine intake, stress and anxiety management, lack of physical activity, and more. Working with a functional medicine provider who can take a 360-degree view and refer you to specialists, if needed, will make all the difference in tackling your sleep problems.
Frequently Asked Questions (FAQs)
Why do I feel so exhausted after 8 hours of sleep?
While sleep duration (or the time you spend asleep) is important, sleep quality (a measure of how refreshing sleep is) matters too. Consider if something is affecting your sleep quality, including poor sleep hygiene, lack of physical activity or light exposure during the day, a bed partner or pet that interrupts your sleep, or underlying health conditions like chronic pain, among other factors.
Why am I still tired after a good sleep?
Your sleep may not be as good as you think. Even if you’re in bed for the recommended seven-plus hours per night, you may be getting restless, not relaxing sleep. Start with a few habit changes, such as sticking to a consistent bed and wake times, getting outside for a half hour per day, staying physically active, and eliminating things that are disrupting your sleep like loud noises or light exposure during the night.
Why do I wake up tired and no energy?
Unfortunately, you’re probably not getting great sleep. See a healthcare provider to look at possible underlying health conditions or undiagnosed sleep disorders that can disrupt your sleep, such as sleep apnea or hormonal changes.
Can getting 8 hours of sleep make you more tired?
Although the general recommendation is that adults should get at least seven hours of sleep per night, everyone’s sleep needs are individual. Meaning, that some people thrive on more, and some function well on less. However, getting eight hours of sleep should not result in fatigue. If you feel like this is going on, you may not be getting eight hours of sleep. Instead, there may be things that are disrupting your sleep throughout the night.
If you’re questioning ‘why am I still tired after eight hours of sleep,’ remember that good sleep is about more than the hours you’re in bed. It’s the culmination of little habits and behaviors throughout the day that add up to good (or poor) sleep. Fortunately, you’re not stuck there. If you’re sleepy throughout the day, it’s a great time to explore all of the potential underlying factors, from health conditions and sleep disorders to sleep hygiene habits and stress management. A functional medicine provider, like one at Parsley Health, can work with you to look at all of these many factors and devise a whole-body approach to sleeping better and feeling better.
Key Takeaways
Sleep quality is a critical component of how well-rested and refreshed you feel when you wake up and throughout the day.
Many things impact your sleep quality, including consistency in wake-up times, exercise habits, nutritional status, mood problems and anxiety, hormonal changes, and more.
Working with a provider to identify the factors that may be impacting your sleep is the first step in creating a better sleep plan. This may include testing to look at your hormones or nutritional status, using a sleep diary to track sleep patterns, or screening for mental health disorders.
Good, refreshing sleep is achievable. Once you get yourself there, you’ll enjoy more energy, better mental clarity, a more stable mood, among many other wonderful benefits.


