If you’re experiencing a runny nose, itchy skin, and trouble breathing, you may think allergies or a cold are to blame. Mast cell activation syndrome (MCAS) probably wouldn’t come to mind, but it can cause these symptoms too.
MCAS is estimated to be present in 17% of the world’s population. Despite its prevalence, the condition is often misdiagnosed because symptoms are similar to other conditions. Understanding when MCAS may be at play (and why it occurs) could be the difference between a right and wrong diagnosis. Ahead, discover the seven root causes of mast cell activation syndrome and what to do if any symptoms associated with MCAS pop up.
What is mast cell activation syndrome?
“Mast cell activation syndrome (MCAS) is a disorder where mast cells, a type of immune cell, release excessive amounts of chemicals, leading to widespread body inflammation and allergic-like symptoms,” says Simon Faynboym, M.D, the medical director of South Torrance Psychiatry Clinic.
When operating business as usual, mast cells play an essential role in our immune system. If a harmful outside substance comes into contact with mast cells, these cells trigger what is known as an inflammatory cascade, a complex sequence that allows the body to heal from allergens or tissue injuries. The response triggered by mast cells is often referred to as an allergic reaction, which sounds ominous but is helpful in eliminating allergens from our body (in moderation).
The trouble comes when mast cells inapproirately prompts this reaction without a clear allergen or trigger. MCAS occurs when these mast cells become defunct and trigger reactions due to internal signals or spontaneously. The body responds as if there is an allergy or infection to fight off, but the response is unnecessary and prolonged.
Dr. Faynboym notes that this condition has far-reaching impacts, and symptoms can be experienced in the skin, gastrointestinal tract, and nervous system. Because of the wide-reaching symptoms and confusion about what triggers the condition, diagnosing MCAS can be difficult.
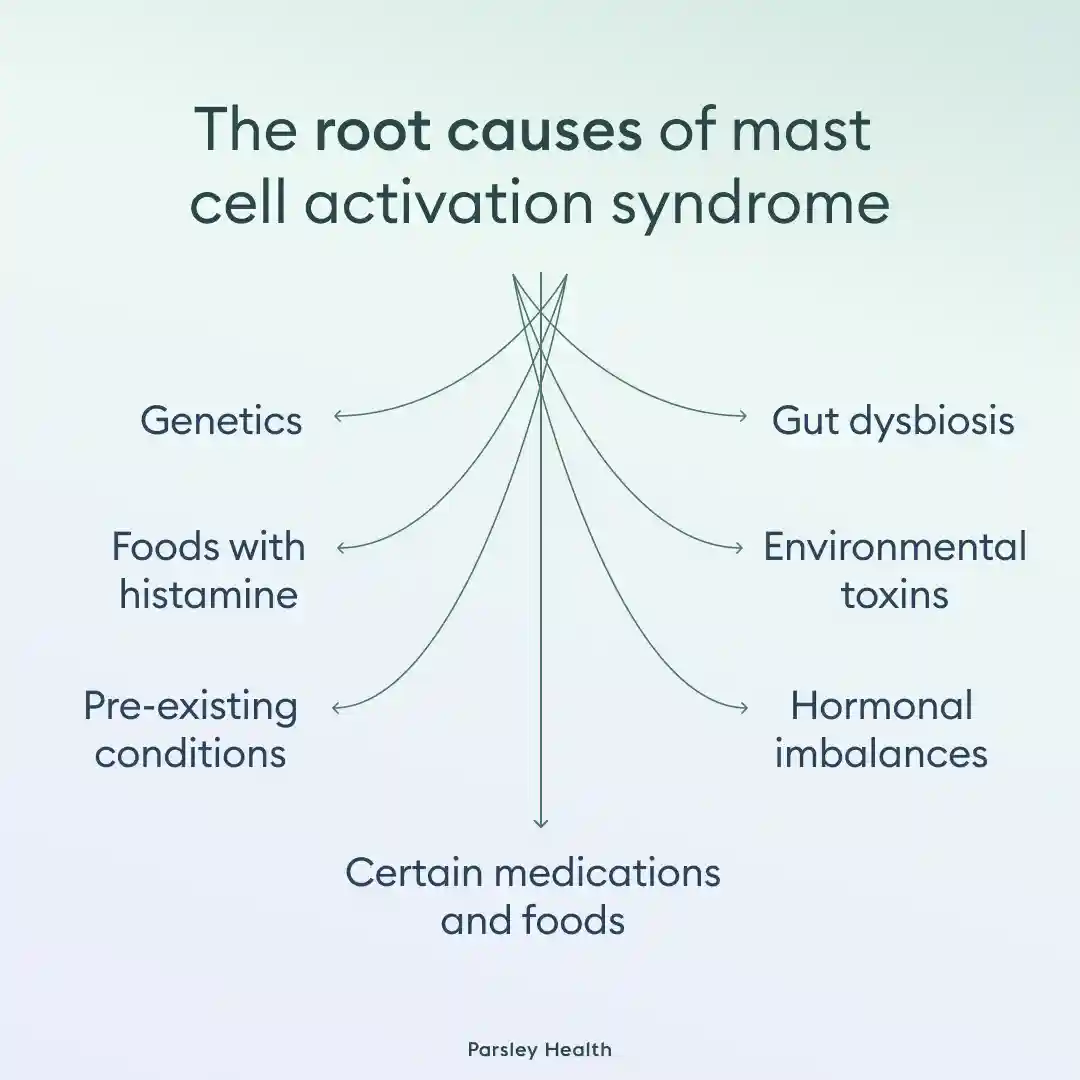
The 7 root causes of mast cell activation syndrome
We all have mast cells, but not all of us develop MCAS. To make matters more confusing, there isn’t a single reason for MCAS disease, but multiple potential ones. Below, we’ve outlined seven of the most common root causes.
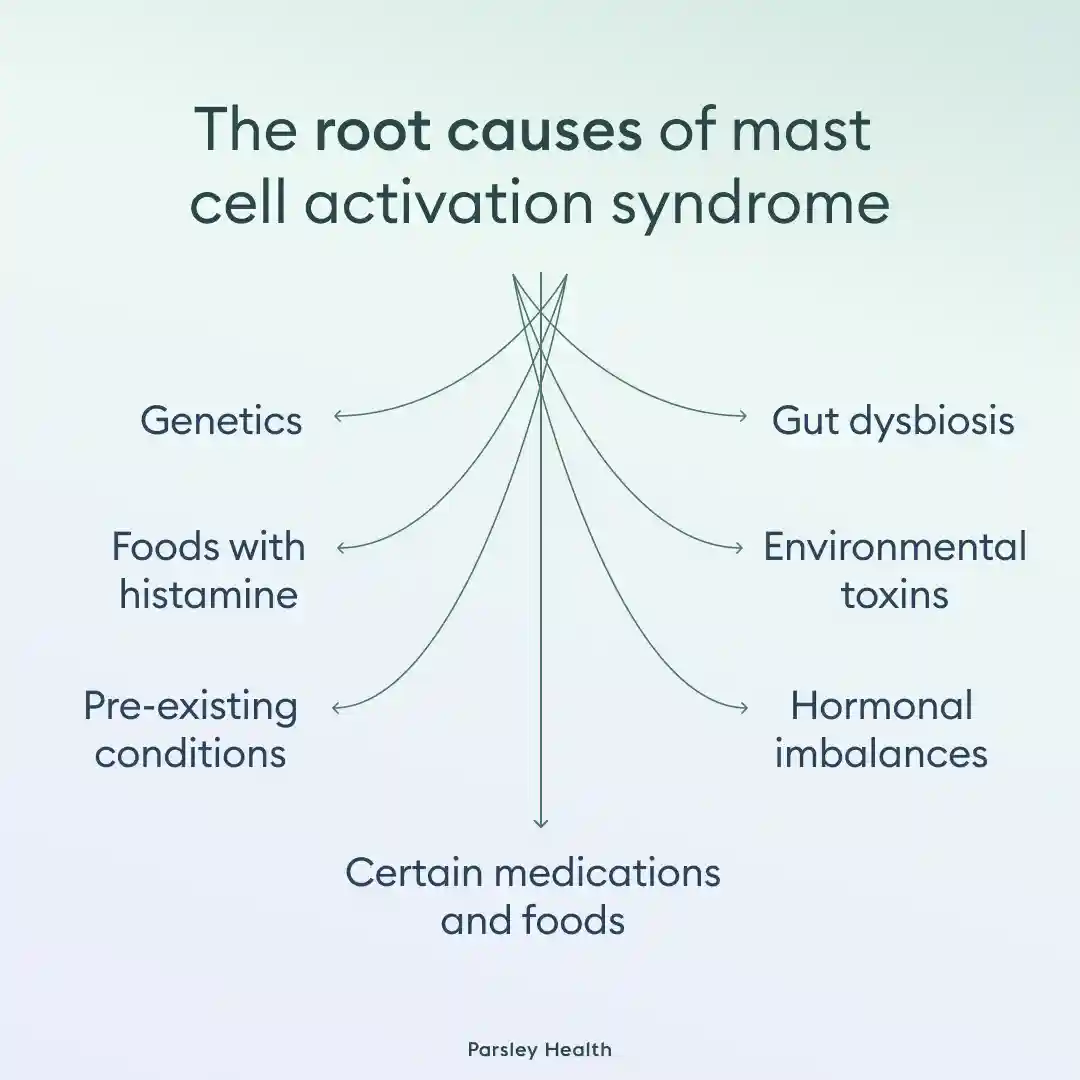
Genetics
As the name suggests, this syndrome occurs at the cellular level. Our cells are heavily influenced by genetics, and scientists have pinpointed certain hereditary conditions that can cause MCAS. Genetics are the most common reason for MCAS, and a few specific conditions can cause MCAS.
One of the most common is hereditary alpha tryptasemia. Those with this condition have multiple copies of the alpha-tryptase gene, a gene that determines the amount of trypase protein in the blood. In turn, these gene copies lead to mast cell dysfunction. A 2021 study suggests this condition is more common in individuals with MCAS than in the general population.
Other genetic conditions linked to MCAS include mastocytosis (a rare genetic condition where someone has too many mast cells) and atopic diathesis (a genetic predisposition to allergies, eczema, and asthma).
Foods with histamine
You are what you eat—and your mast cells may be reacting to your meals as well. Histamine-releasing foods have been linked to MCAS flare-ups. These include:
- Alcohol
- Processed meat
- Certain cheeses
- Tropical fruits, like pineapples, papaya, and citrus fruits
- Eggplants
- Spinach
- Tomatoes
- Shellfish
- Strawberries
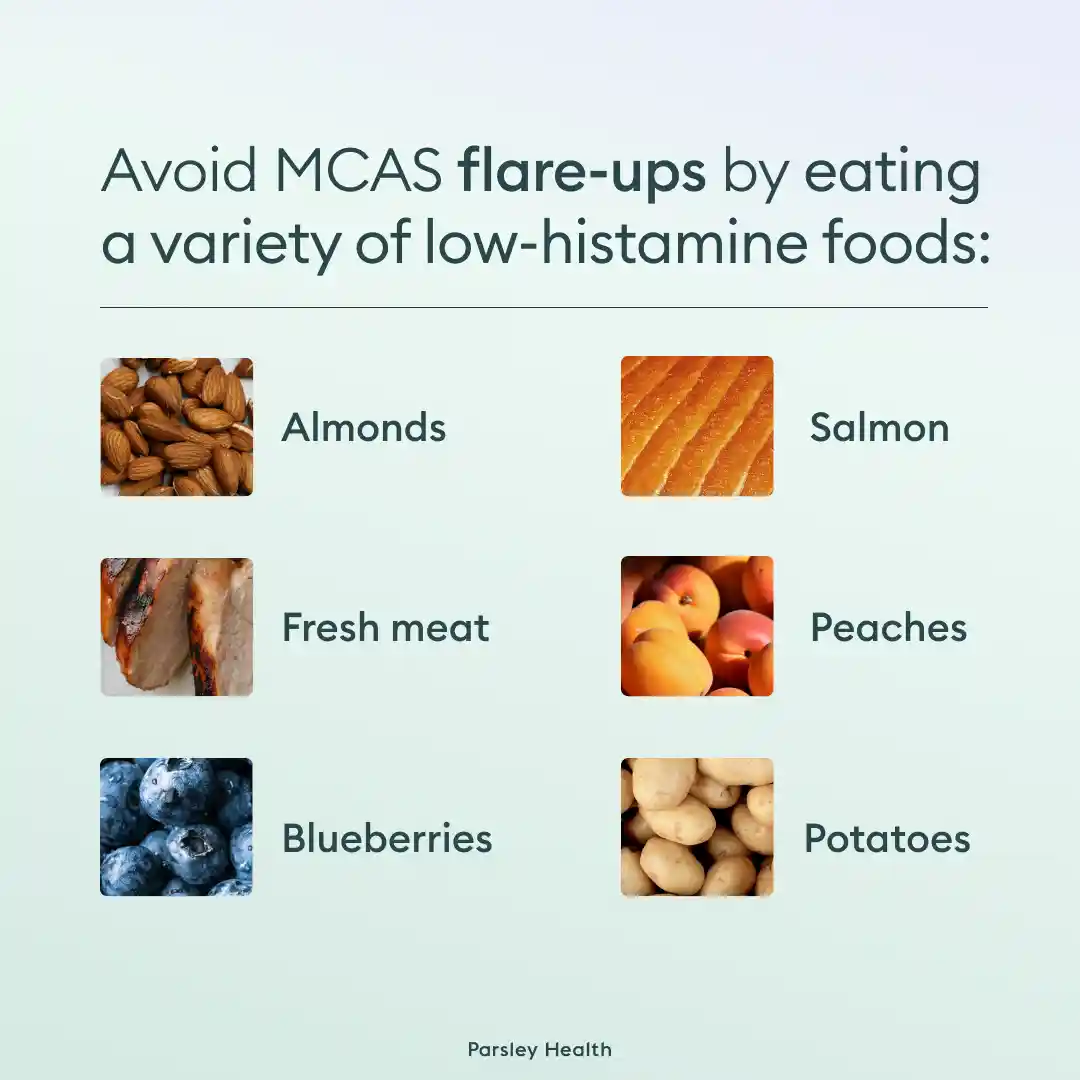
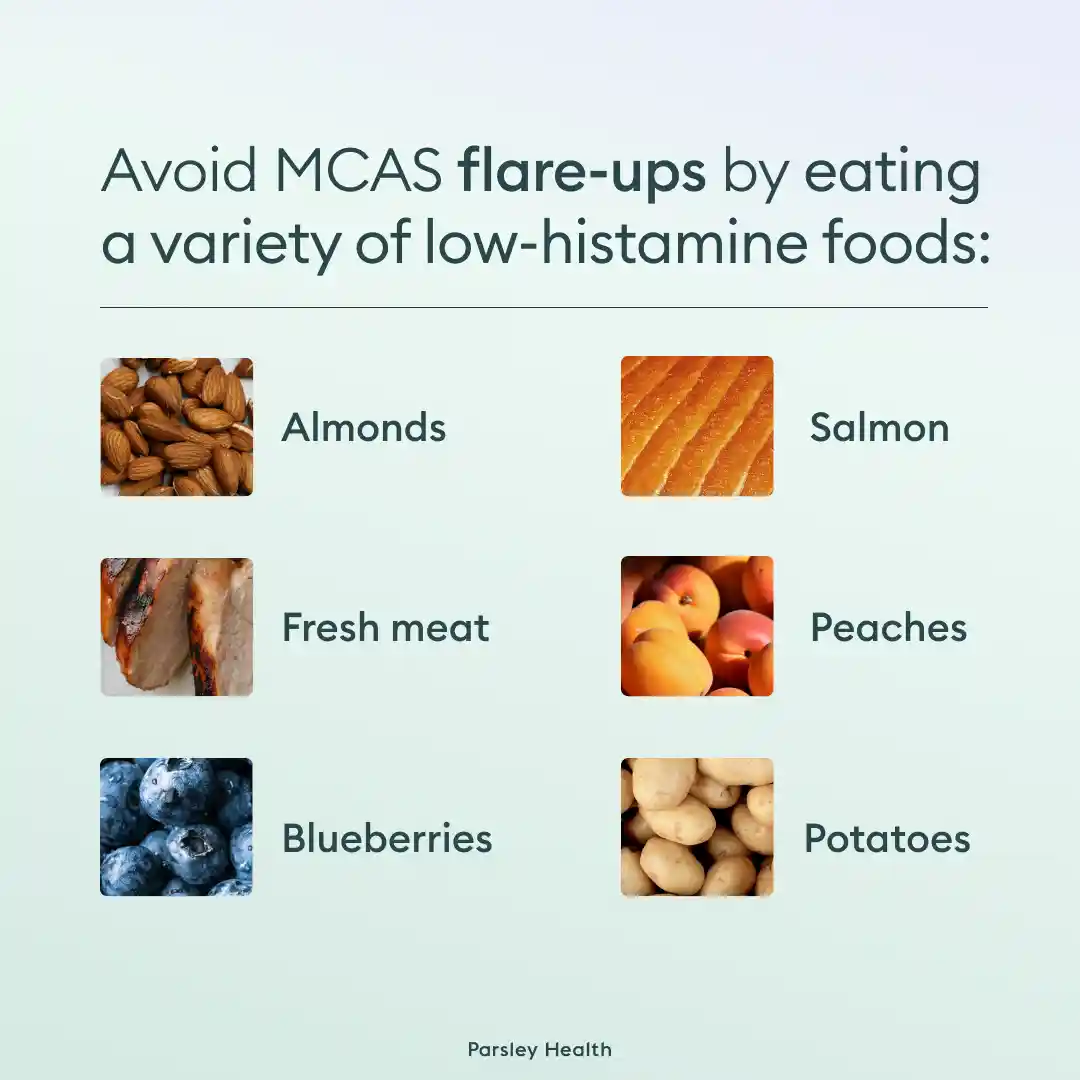
When foods are a trigger, someone may benefit from the low histamine diet. The name for this diet was chosen carefully and should not be interpreted as a no histamine diet, which could lead to nutritional deficiencies. Instead, the low histamine diet aims to discover which high histamine foods trigger MCAS symptoms so they can be avoided or consumed in moderation.
Pre-existing conditions
Individuals with certain conditions are more likely to develop MCAS. These pre-existing conditions fall into two camps: disorders impacting mast cells directly and mental health conditions. The first includes genetic conditions we already discussed (to recap: hereditary alpha tryptasemia, mastocytosis, and atopic diathesis).
The second is mental health conditions, including OCD, ADHD, anxiety, and depression. Unlike the first category, these conditions have a complicated relationship with MCAS; often it’s a chicken and egg scenario where it’s unclear if the mental health conditions or MCAS developed first.
“These mental health conditions may either develop as a result of chronic inflammation caused by mast cell activation or exacerbate MCAS symptoms due to heightened stress and anxiety levels,” explains Dr. Faynboym, “Stress-related mental health conditions can create a cycle where increased mast cell activation worsens mental health, further triggering mast cell release.”
It’s important to note that mental health conditions and MCAS may go hand-in-hand because they stem from the same genetic variataions. The genes involved in the three genetic conditions above can also impact mental health.
Gut dysbiosis
Our gut plays a major role in the likelihood of a MCAS diagnosis. If someone experiences gut dysbiosis, an imbalance in the gut microbiome, they are more likely to develop MCAS.
When our gut microbiome is imbalanced, there are more histamine-secreting bacteria in it. These bacteria then trigger mast cell reactions (remember: part of the mast cells’ job is to respond to histamine in the body), sometimes resulting in MCAS. Researchers are still studying the relationship between gut imbalances and MCAS, meaning there’s a lot that we don’t yet understand about this cause.
Stress
“From my background in procedure-based specialties like ER and urgent care, I've observed that stress and anxiety can worsen by increasing stress hormones, like cortisol, which contributes to inflammation and can exacerbate the symptoms,” says Holly Town, PA-C, a physician's assistant at Aqua Body Lab.
Dr. Faynboym explains this connection, “Stress activates the release of various hormones and neuropeptides like corticotropin-releasing hormone (CRH) and substance P, which can directly stimulate mast cells. This leads to the release of inflammatory mediators such as histamine, exacerbating MCAS symptoms.”
He adds that chronic stress has been linked to too much mast cell activity, which can lead to MCAS as well as systemic inflammation. In one small-scale study, patients with MCAS commonly reported chronic stress and that stressful moments triggered their MCAS symptoms.
Certain medications and foods
Some medications can cause hyperactivity in mast cells, leading to MCAS. These include opiates, non-steroidal anti-inflammatory drugs, muscle relaxants, and some antibiotics, including quinolones. Valproic acid, a medication that treats bipolar disorder, has also been linked to MCAS.
If you start to develop any MCAS symptoms while on these medications, it’s best to consult a healthcare provider who can make a proper diagnosis and adjust medication as necessary.
Environmental toxins
“Environmental factors, like pollutants and allergens, play a significant role in MCAS,” says Town. Over the past 50 years, there has been an increase in patients with MCAS, but not in the genetic conditions linked to this disease. This has led scientists to investigate the role toxins have in MCAS development.
Three toxins often linked to MCAS include:
- Bisphenol A (BPA): A chemical found in many plastics, including water bottles, food storage containers, and children’s toys.
- Aflatoxin B: A fungal toxin that can be in nuts, rice, figs, and other foods.
- Benzo(a)pyrene: A carcinogenic found in tobacco, some foods, and car exhaust.
Hormonal imbalances
Last but not least: MCAS can be caused by hormonal imbalances. Stress, for example, causes a cortisol imbalance and has been linked to MCAS. But cortisol isn’t the only hormone known to cause this syndrome.
Emerging research suggests two female sex hormones, progesterone and estradiol, also influence the behavior of mast cells. If either (or both) of these hormones are imbalanced, the chance of developing MCAS increases. This may also explain why women with MCAS have female-specific symptoms, such as period pain or heavier menstrual flows.
MCAS treatment options
Often, the hardest part of treating mast cell activation is getting the correct diagnosis. Once diagnosed, there are multiple effective treatment options. For maximum impact, it’s encouraged to mix and match treatment types.
“Treatment typically involves directly reducing mast cell activation using medications such as antihistamines, alongside lifestyle changes to avoid known triggers,” explains Dr. Faynboym. He emphasizes that treatments should address both physical and psychological symptoms in order to be effective.
Specific antihistamines that may be prescribed include type 1 receptor blockers, especially if itching or redness occurs. Diphenhydramine and hydroxyzine are two common type 1 receptor blockers. If side effects from this class of medications are too severe, second generation antihistamines, like loratadine, cetirizine, and fexofenadine, may be prescribed. Aspirin may also help reduce flushing or headaches caused by MCAS. In severe cases, corticosteroids are prescribed.
But these medications are better at treating side effects, not at preventing future symptom flare-ups. To address the root causes of MCAS, lifestyle changes should be undertaken—but more on that in the next section.
Lifestyle changes to treat MCAS
“Several lifestyle and mental health interventions can help manage MCAS symptoms,” says Dr. Faynboym. He often recommends cognitive behavioral therapy, stress management techniques, and mindfulness to patients with MCAS. Adjustments to diet and your sleep routine can also help.
Low-histamine diet
As we’ve discussed, the low-histamine diet may help identify foods that trigger MCAS. Histamines are found in a variety of foods, including healthy options like spinach, strawberries, and bananas.
However, getting rid of all foods containing histamine would lead to nutritional deficiencies. While citrus fruits and fermented foods may trigger the most histamine-related symptoms, specific triggers differ from person to person. To discover your specific food triggers, you can undertake a low-histamine diet (with the supervision of a qualified healthcare provider). Once triggers are discovered, they can be avoided or enjoyed in limited quantities, with the help of supplements that break down histamine.
Stress reduction
Stress is one of the most common (and controllable) MCAS triggers. Town explains, “It's essential to focus on reducing stress to better manage this condition.”
Effective stress reduction techniques include:
Additionally, Dr. Faynboym adds that those with MCAS may benefit from CBT or mindfulness-based therapy with a licensed mental health provider.
Sleep support
Your circadian rhythm, the body’s internal clock, can impact the severity of MCAS symptoms. When our sleep patterns are out of rhythm, symptoms often worsen. Good sleep hygiene habits can restore that healthy circadian rhythm, reducing MCAS flare-ups.
Specific habits to implement include:
- Go to sleep and wake up around the same time each day
- Avoid “social jet lag,” also known as having different sleep patterns during the work week and on days off
- Create a dark, quiet sleep environment
- Walk or stand in sunlight during the day
- Have a regular exercise and eating schedule
Frequently asked questions (FAQs)
What vitamin deficiency causes mast cell activation?
Some evidence suggests that a vitamin D deficiency may cause mast cell activation syndrome. Vitamin D supports healthy immune system function, among other health benefits. We get Vitamin D through direct sunlight, supplements, and certain foods, including eggs yolks, oily fish, and fortified foods.
What mental illness is associated with mast cell activation syndrome?
Multiple mental illnesses are associated with mast cell activation syndrome. These include anxiety, depression, ADHD, and OCD. Stress has also been linked to MCAS.
What drugs should be avoided in mast cell activation syndrome?
Drugs that often trigger MCAS include non-steroidal anti-inflammatory drugs, opiates, and muscle relaxants. Certain antibiotics, including quinolones, and valproic acid, a medication that treats bipolar disorder, have also been linked to MCAS.
What stops mast cell activation?
Stopping mast cell activation often requires lifestyle interventions combined with medications and supplements to treat flare-ups. Commonly prescribed medications include antihistamines and aspirin. Lifestyle interventions include getting regular exercise, regulating stress, and developing healthy sleep habits. A low histamine diet and therapy may also help stop MCAS.
Which antihistamine is best for mast cell activation syndrome?
Two classes of antihistamines are commonly prescribed for MCAS: type 1 receptor blockers and second-generation histamines. The first may be more effective, but the latter has fewer side effects and may be better tolerated.
How to cure mast cell activation?
There isn’t a “cure” for mast cell activation syndrome, though if it is caused by gut dysbiosis, it can be resolved by taking care of gut health. Instead, treatment revolves around managing symptoms and identifying and avoiding triggers. For the former, antihistamines or aspirin are commonly prescribed. Lifestyle interventions, like exercise, a low histamine diet, and stress reduction techniques, can help with the latter.