We all know stress plays a big role in our overall health, but can being stressed make you sick? It turns out, the answer is yes. Prolonged stress weakens the immune system and can exacerbate chronic conditions like multiple sclerosis and diabetes.
So you had a rough week at work, an argument with your partner, you’re attempting to focus on your third Friday Zoom call in a row, and you feel a cold coming on. Sound familiar? If you’ve experienced stress and sickness at the same time, you’re not alone. But can stress actually make you sick, or is it just a coincidence?
While the term “stress” might sound benign, in reality stress is anything but harmless—especially when it becomes chronic. Chronic stress can weaken your immune system, increase inflammation, and dysregulate your hormones. Which, in turn can lead to a variety of short-term and long-term illnesses.
What is stress?
“Essentially, stress is a response to a threat,” says former Parsley Health provider Jamie L. Guyden, MD. She explains that this threat might be real and immediate (being chased by a bear) or perceived (speaking before a large group). In both cases, you may experience the same psychological and physiological reactions, regardless of whether you’re actually facing a dangerous situation or not.
When you perceive a situation as stressful, your hypothalamus, a gland at the base of your brain, activates your sympathetic nervous system (SNS), or the fight-or-flight response. When it turns on, your brain releases epinephrine (also known as adrenaline) and norepinephrine, which are hormones. You might notice a temporary increase in your heart rate and blood pressure, along with increased alertness and decreased digestion and urine production. This is your body’s way of diverting your energy toward managing the stressor, says Dr. Guyden.
Simultaneously, your adrenal glands release cortisol, the primary anti-inflammatory stress hormone, to release glucose (sugars) into your bloodstream so you can take quick action. “Cortisol will also activate the inflammatory cascade in an effort to aid in tissue repair and recovery,” explains Dr. Guyden. Once the stressor recedes, your body should return to homeostasis. This reaction “is designed to be short-lived,” she explains.
Acute vs chronic stress
At times, we all experience short-term stress. Sometimes, it can be a powerful motivator, inspiring us to work harder on a passion project or push ourselves during a workout. But when the stress response remains activated for a prolonged period, you’re at risk for chronic stress—and chronic stress is never good.
According to Dr. Guyden, chronic stress results when there are multiple sources of stress that you’ve been experiencing for three months or more. This leads to sustained activation of the body’s stress system, the Hypothalamic-Pituitary-Adrenal Axis (HPA axis), which releases stress hormones.
Can stress make you sick?
Chronic stress provokes your immune response, sending chemicals known as pro-inflammatory cytokines to attack the threat. Over time, Dr. Guyden says, your body can become cortisol-resistant, which means your inflammation response never shuts off. Chronic inflammation like this can lead to a number of serious health conditions, and it can impact your immune system.
Over time, stress' negative impact on the HPA axis can dysregulate your hormones and lead to changes in your immune system that can make you more susceptible to illnesses and chronic conditions.
Common signs that stress is making you sick
We all feel stress at times, but how can we tell when stress is making us sick? There are a few telltale signs, including:
Changes in sleep patterns
Experiencing more headaches than usual
Frequent illnesses
Lack of energy
Muscle soreness
Persistent fatigue
Prolonged recovery times
Worsening of pre-existing health conditions
It’s important to note that all these signs could be due to a different underlying cause. A functional medicine provider can help you determine the root cause. Whether it’s stress or something else, they’ll also work with you to develop a treatment plan.
Physical effects of chronic stress
“Our brilliant bodies are designed to respond to stress,” says Dr. Guyden. However when prolonged or multiple stressors suppress the parasympathetic nervous system, you may experience a variety of chronic stress symptoms.
The long-term activation of the HPA axis and elevated cortisol levels can cause physical symptoms of stress, including:
Chronic pain
Dizziness/fainting
Digestive problems
Fatigue but difficulty sleeping (a.k.a. “wired but tired”)
Increases in blood pressure, cholesterol, and heart disease
Increase in blood sugar levels
Lowered immune function
Memory issues
Mood disturbances such as depression, anxiety, or irritability
Muscle tension
Weight gain
Urinary problems
“Interestingly, with long-term chronic stress, cortisol may eventually decrease, causing chronically low cortisol, leading to a slightly different picture,” says Dr. Guyden. Symptoms of this can include:
Craving salt and spicy foods
Diminished motivation
Hormonal issues such as early menopause or low libido for women
Low blood pressure
Morning fatigue
Panic
Poor concentration
This might appear to be a long list of unrelated symptoms, but Dr. Guyden has an explanation: “Chronic stress can affect any organ or gland in the body, as our hormonal system works through a sophisticated symphony throughout the body, heart, and mind.”
Long-term impact of stress
Chronic stress not only suppresses your immune system functioning in the short-term; it can also increase the risk of developing multiple chronic conditions and high blood sugar.
Altered immune function
Although cortisol is anti-inflammatory and typically suppresses pro-inflammatory cytokines, chronic cortisol elevation can result in a “resistant” immune system. This comes along with an accumulation of stress hormones; this creates an inflammatory response that further depresses the immune system.
Altered immune function due to HPA axis dysregulation has been shown to exacerbate irritable bowel syndrome and multiple sclerosis, among other chronic conditions.
Cardiovascular health
Cortisol due to stress can cause narrowing of the arteries, plus the release of epinephrine to increase your heart rate and pump your blood harder. Like all hormones, cortisol is made from cholesterol. Therefore, “chronic cortisol elevation will require more precursor and thus cholesterol production,” says Dr. Guyden.
Increased cortisol levels can result in elevated cholesterol, high blood pressure, and elevated triglycerides. Elevated cortisol can also cause changes that encourage the buildup of plaque in the arteries and abdominal adiposity, or belly fat. All of these factors increase the risk of cardiovascular disease, including heart attack, stroke, heart failure, and arrhythmia.
Blood sugar dysregulation
During the stress response, the release of cortisol triggers the release of glucose, giving your muscles a burst of energy—which you’d need in order to, say, run from a burning building. But if you’re just anxiously stuck in traffic, that excess sugar circulates through your bloodstream, leaving you with high blood sugar. Cortisol also inhibits the release of insulin, which is the hormone responsible for regulating your blood sugar.
Because of this, chronic stress can lead to chronic high blood sugar, which creates problems even if you don’t end up with Type 2 diabetes. Such problems can include:
Dry mouth
Dizziness/lightheadedness
Frequent urination
Increased thirst
Nausea/vomiting
Weight gain
If you do develop Type 2 diabetes, chronic stress can bring on complications, such as neuropathy, retinopathy, kidney disease, and macroangiopathy.
Mental and emotional impact of chronic stress
Chronic stress’ impact doesn’t end with your physical health. It can also instigate long-term changes to your emotional health, such as the development of depression and anxiety, and may cause brain fog and other cognitive symptoms of stress.
Stress and the increased risk of anxiety, depression, and mood disorders
Chronic stress dysregulation of the HPA axis can lead to a drop in dopamine and serotonin, which adversely affects your mental health. A recent poll suggests that 53% of Americans experience chronic stress. A 2020 study in Brain, Behavior, and Immunity, found that chronic stress induces a pro-inflammatory cellular response in the brain, potentially triggering anxiety, depression, and mood disorders.
Cognitive effects: brain fog, memory issues, and trouble concentrating
According to Dr. Guyden, many people with chronic stress report feeling “wired but tired.” In other words, you might feel exhausted, but when your head hits the pillow, you struggle to fall asleep. When the HPA axis is dysregulated by chronic stress, it’s not uncommon to experience unrelenting fatigue. Research shows elevated cortisol levels can inhibit REM sleep and cause interrupted sleep.
Chronic stress can also interfere with cognition, causing “brain fog ” or difficulty with memory and concentration. A 2022 study found that participants who experienced higher levels of perceived stress experienced cognitive effects like trouble concentrating or mental fatigue.
How to identify personal stress triggers
It’s important to note that the same circumstances may elicit the fight-or-flight response in some individuals but not others. “Some people find excitement in small amounts of stress, and thus, their bodies don’t respond to them as ‘stressful,’ and potentially, have no physiological response,” says Dr. Guyden. “Others, depending on multiple factors, including, but not limited to, lifestyle, socioeconomics, childhood trauma, and genetic factors, respond to very small stressors as if they are life-threatening.”
To identify your own stress triggers, think through different situations that cause you to worry at work, at home, or in social situations. Health and finance are also arenas where stress is a frequent visitor. If you struggle to pinpoint triggers right away, you’re not alone. Many people (myself included) find that journaling about day-to-day life or reflecting on emotions through meditation makes it easier to identify what, exactly, is causing stress.
How to manage and reduce chronic stress
Once you’ve identified triggers, it’s time to make a plan to manage chronic stress—and that plan begins today, not sometimes in the future. “We shouldn’t be waiting until we are in emergent states of health to address the chronic stressors that many of us face,” says Dr. Guyden. This is particularly true if you have high blood pressure, high cholesterol, or diabetes. “As we’ve learned, these are diseases of stress and should be addressed holistically,” she explains.
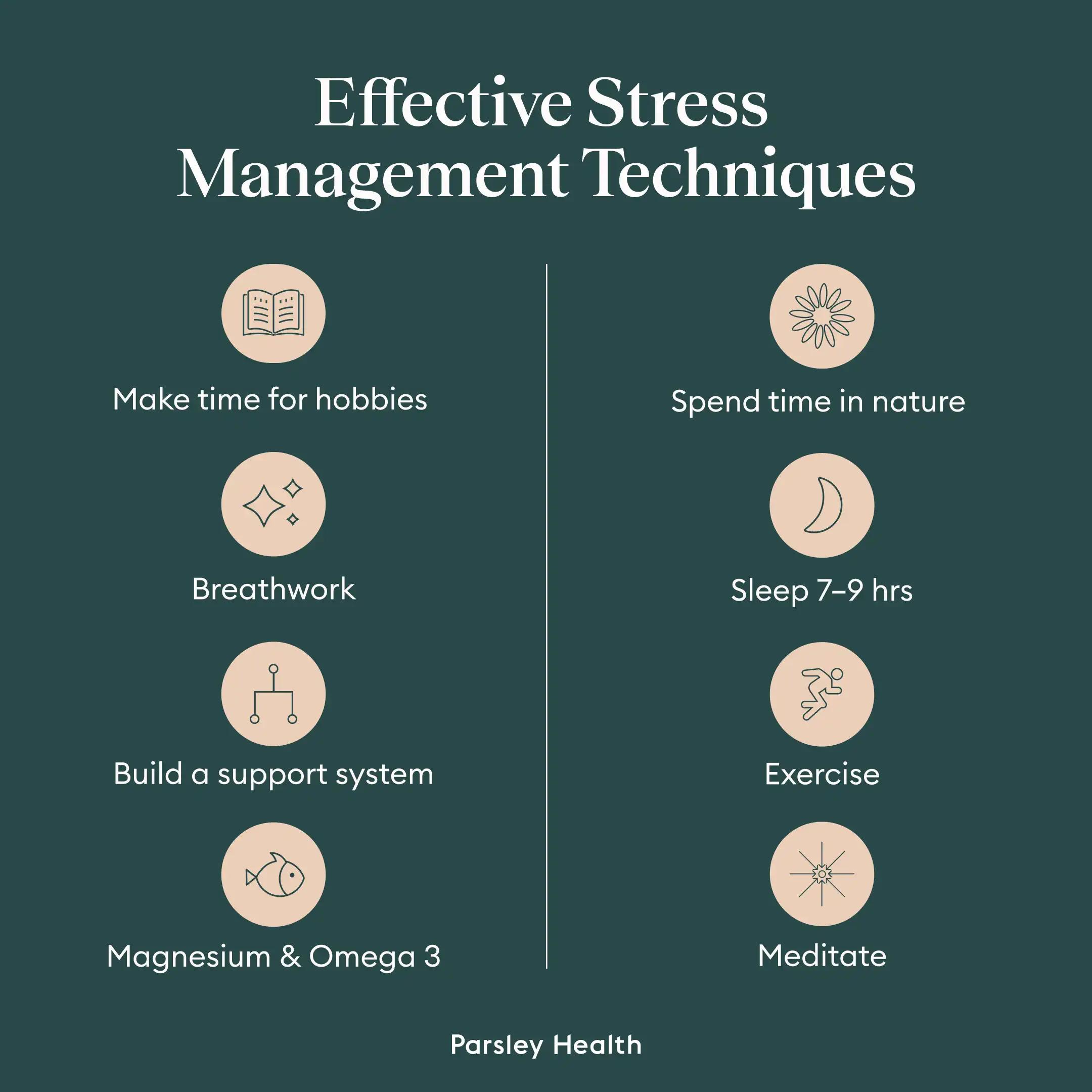
Some of the most effective stress management techniques include:
Breathwork (this video is great for beginners to the practice)
Building a support system, whether it consists of loved ones or a formal support group
Exercise (and pick your poison: low, medium, and high-intensity workouts can all lower stress levels!)
Make time for hobbies you enjoy, whether that’s needlepoint or playing piano
Meditation, whether guided or simply setting a time and sitting in silence
Sleeping seven to nine hours a night
Spending time in nature
Making sure your diet is rich in magensium, omega 3 and anti-inflammatory
If you’re like me and want a structured program to follow, consider creating a cortisol detox, either alone or with the support of a functional medicine provider. Many people also find it useful to talk to a mental health professional, who can provide support and expert strategies personalized to your situation.
When to seek medical advice
Anyone experiencing chronic stress may benefit from seeing a functional medicine doctor and health coach, such as the ones at Parsley Health. A functional provider can address the root cause of your health problems, not just the symptoms. “By connecting an individual with where and how chronic stress has crept in, understanding one’s response to stress, how an individual restores and rejuvenates and what long-term traumas, emotional stressors an individual has perceived,” says Dr. Guyden, “we are able to create a pathway to reversal.”
Key takeaways
The verdict is in: Stress can make you sick, thanks to its impact on the HPA axis and immune system. When stress becomes chronic, it also increases the risk of conditions ranging from diabetes to heart disease. If you’re experiencing chronic stress, remember:
Stress impacts your health: Chronic stress can leave a lasting mark on your physical, mental, and emotional health.
Identify stress triggers: It’s in your control to manage and reduce your chronic stress levels. The first step to do so is to identify your triggers.
Reduce stress: After identifying triggers, you can brainstorm ways to avoid them when possible, plus practices that can help manage your stress, such as meditation and exercise.
For help creating a personalized stress detox plan, work with a functional medicine provider. The providers at Parsley Health regularly help members reduce stress levels naturally and get to the root cause of any sicknesses. Reach out today for a consultation.
Frequently Asked Questions (FAQs)
Can stress make you feel sick physically?
Stress can indeed make you feel sick physically. Physical symptoms of stress include muscle aches and pains, nausea, dizziness, and lowered immune function.
What are the physical symptoms of stress?
The physical symptoms of stress are far-reaching since stress impacts our entire body. The most common physical stress symptoms include fatigue, muscle aches, chronic pain, difficulty sleeping, dizziness, weight gain, digestive issues, and urinary problems.
Can stress cause flu-like symptoms?
Since stress can weaken the immune system, it may make the body more susceptible to viruses that cause flu-like symptoms.
Can stress cause you to throw up?
Stress doesn’t typically cause someone to throw up, but it can in severe cases. Chronic stress impacts our entire body, including the digestive system. When stress is persistent or sudden and intense (think: a panic attack), someone may vomit.
How to stop being sick from stress?
If you’re sick from stress, it’s not a chicken-and-egg situation; the stress is usually the root cause. To reduce your stress, identify any triggers in your life and either remove them or come up with a plan about how to respond when a trigger pops up. Adding in some stress-reducing habits, like meditation or journaling, can also be beneficial.


