There’s nothing more frustrating than getting sick and having trouble finding answers to the reason behind your symptoms. But this is often the case for people who suffer from autoimmune disorders, a type of illness where the immune system is triggered to attack your body. Common autoimmune diseases include Hashimoto’s thyroiditis, rheumatoid arthritis, and inflammatory bowel disease. There are more than 80 known autoimmune conditions, and they disproportionately affect women. Of the 8% of the population that are affected by autoimmune disease, women account for 75% of all cases.
And those numbers could underestimate the number of people actually impacted by autoimmune disease. Unfortunately, these disorders can be tricky to diagnose and treat, especially in the conventional medicine approach, where doctor visits last only around 20 minutes, and most people only speak for 11 seconds before their doctor cuts them off.
Because autoimmune disorders aren’t always straightforward, they take time and patience to diagnose and treat. Without that, many people find that they have been misdiagnosed, or feel debilitating symptoms and reach dead ends when looking for solutions.
Below, Lilli Link, MD, a doctor at Parsley Health, explains why autoimmune disorders are easy to miss in conventional medicine practice and how a root-cause medical approach can be used for autoimmune disease treatment and diagnosis.
Why are autoimmune disorders hard to diagnose?
There are several reasons why autoimmune diseases can be tricky to diagnose. First, many of the symptoms that can point to autoimmunity could be attributed to several other causes, which is why many doctors can brush them off initially.
“Autoimmune disorders can get missed because the symptoms aren’t always clear-cut. Because some people will feel fatigued, or they will feel some joint pain and the joint pain moves, or they have a rash and it’s hard to diagnose because it’s not a classic rash—the signs of it can be somewhat nebulous,” Dr. Link says.
Some of the symptoms like fatigue and brain fog will not automatically make a doctor think “autoimmunity.” But even if you do have classic autoimmune disease symptoms like rheumatoid arthritis, for example, once a doctor performs an antinuclear antibody (ANA) test, the primary test for evaluating autoimmune disorders, there is a chance that the test may not read positive—even if you really do have an autoimmune disease.
“The testing isn’t perfect. You can test for autoimmunity and sometimes it’s clear that somebody has classic symptoms. But there’s such a thing as seronegative rheumatoid arthritis,” explains Dr. Link, “So somebody could have the symptoms but none of the tests show they have it, but they get that diagnosis anyway. Or people will have positive antibodies and they have no symptoms that go along with autoimmunity,” she says.
“It’s not like when you break your leg and you can see exactly where the break is. It’s not always that clear-cut. So it’s very easy to miss that diagnosis or be unsure about that diagnosis.”
Not sure what your symptoms are really telling you?
The Parsley Symptom Index helps connect the dots across your whole body so you can understand patterns, not just isolated symptoms.
What causes autoimmune disorders?
Although exactly what causes autoimmune diseases is unknown, it’s likely due to a combination of factors. Genetics do play a role, but so do lifestyle factors like diet, stress, and environment.
According to Dr. Link, when someone develops autoimmunity it’s because the immune system has become “confused.” Normally the job of your immune system is to know when a foreign invader (like a virus or other pathogen) is present and it’s supposed to attack the foreign invader and kill it. But in the case of autoimmunity, the immune system does not recognize the difference between your own body and something it’s supposed to kill, so it attacks itself.
Autoimmunity and stress
A study published in JAMA in 2018 showed a clear link between stress and autoimmunity. Dr. Links also says she’s seen this anecdotally in her own practice. Often a stressful life event or chronic stress can spur the development of the disease. For many patients, they may have a genetic disposition for autoimmunity, but then something happens in their life to trigger the disorder.
“Almost uniformly, I would guess around 99% of my own patients have a family history of autoimmunity. Not every person with a family member with autoimmune disease ends up with it. Usually, it’s something that is spurring on the autoimmune condition to start,” says Dr. Link.
That’s just one reason why Parsley Health doctors like Dr. Link take an in-depth family and health history of members. “We like to understand that person as deeply and completely as we can so that we can get clues about why this is happening. Because it’s not the same for every person,” Dr. Link says.
Dr. Link has seen both physiological and psychological events trigger autoimmune disease in patients. “I have a patient that developed celiac disease around the age of 70 after breaking her jaw. She went 70 years without problems with gluten, but then after that traumatic experience she did,” explains Dr. Link. “I also had someone who had a very bad breakup with a partner and then got Graves’ disease,” she says.
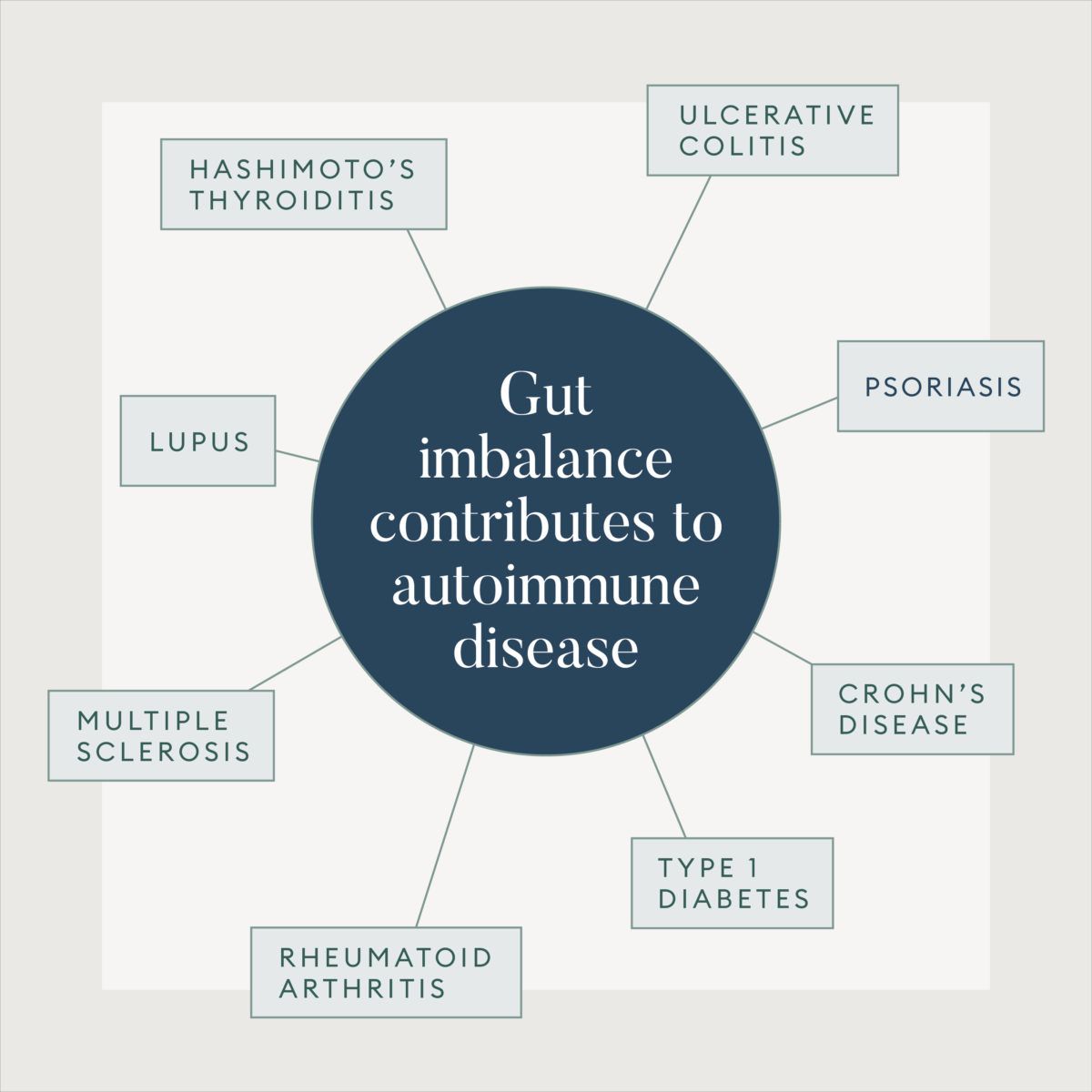
Autoimmunity and gut health
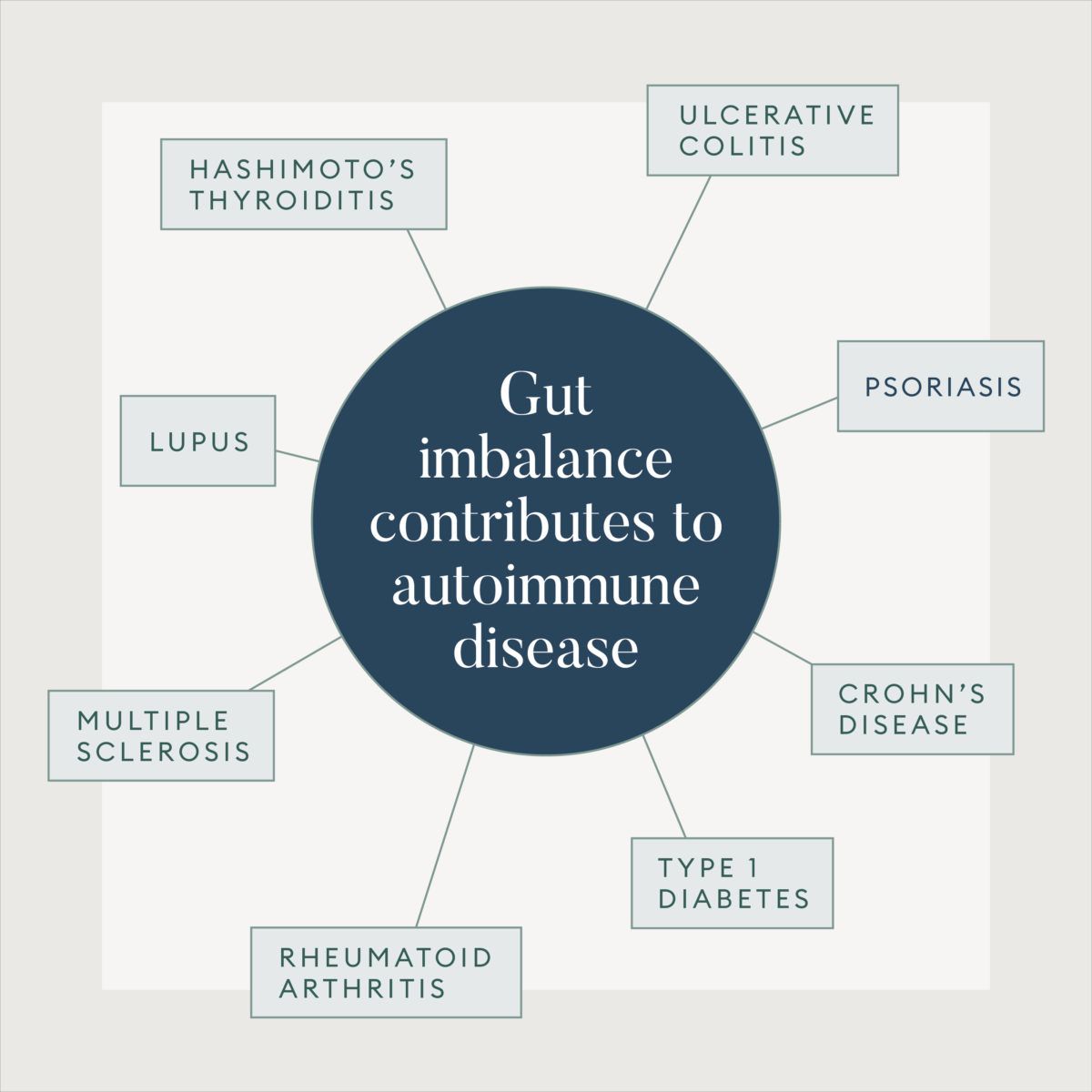
There is also a link between the gut microbiome and autoimmunity, explains Dr. Link. “Leaky gut can create the landscape or opportunity for autoimmune disease to either start or flourish,” she says. Leaky gut is a condition where the gut barrier or lining becomes compromised, and molecules are able to move across the gut barrier into areas they wouldn’t normally be. This can trigger inflammation. Several different things can lead to leaky gut but some of the common factors at play are diet, stress, chemical exposure, and medications. Science also suggests that leaky gut is associated with chronic disease, including autoimmune disease.
Oftentimes, a comprehensive approach to autoimmune disease treatment will involve healing the gut, in addition to addressing other factors like sleep, stress, and diet.
Parsley Health offers physician-led functional medicine care, advanced lab programs, and flexible ways to get started, all designed to help you feel better over time.
Holistic autoimmune disease treatment
Medical providers at Parsley Health use an inside-out approach to autoimmune disease treatment (which we call root-cause resolution medicine) that involves first detecting the illness correctly and then understanding why the immune system got confused in the first place.
Then, your doctor will look at your entire lifestyle in order to begin treating your illness at the root. The goal is to decrease inflammation in the body, balance the immune system, and manage symptoms through a doctor-prescribed health plan with recommendations around diet, exercise, sleep, and more. You’ll receive support from a health coach to help you implement every step of the plan.
Conventional autoimmune disease treatment usually involves treating the symptoms through the use of medication which suppresses the entire immune system. And as presented in a review published in the Indian Journal of Pharmacology, conventional autoimmune disease treatments can fall short of helping people who suffer from them.
Many medications used for autoimmune disease treatment suppress the immune system in totality, explains Dr. Link. “Having a diminished immune system can put you at risk for other problems.”
It’s not that there is never a place for medication—for some cases, it is necessary, especially when all other methods have failed or if someone isn’t able to adhere to lifestyle changes.
“Sometimes there can be a role for medication when you can’t improve the situation by addressing the underlying causes,” Dr. Link says. “But oftentimes you can make a huge difference with somebody if you address the underlying causes.”
Dr. Link notes that if a case of autoimmune disease can’t be controlled well enough with diet, lifestyle, supplements, and other aspects, medication will be needed to prevent further harm. “For example, with rheumatoid arthritis, you can get permanent joint damage. Even if you are taking medication, the goal is to start healing and slowly minimize the medication as much as possible,” Dr. Link says.
The healing process for autoimmune diseases is a process and journey that you will take with your providers, and as life or anything else changes, your plan can change until you feel you have what you need to heal.