Facial eczema is simply eczema that occurs on your face. It involves the same frustrating host of symptoms, such as itching and irritation, and the same triggers that are common with bodily eczema. However, eczema on the face can present additional challenges because skin tends to be more sensitive and exposed to more triggers.
Inflamed, itchy, flaky, irritated skin is frustrating no matter where it crops up. But when eczema shows up on your face, your frustration meter can skyrocket. Facial eczema can be uncomfortable, sure, but it can also tank your confidence and be more complicated to treat.
“One key challenge with facial eczema is the emotional toll it takes because it's so visible,” says Shamsa Kanwal, MD, a consultant dermatologist with myHSTeam. “Patients often experience lowered self-esteem and social anxiety, especially during flares.”
She adds, “The skin on the face is also more delicate and sensitive than other areas, which limits the use of certain medications and requires a more cautious, tailored approach.”
Eczema doesn’t have a cure, according to the National Eczema Foundation. But treatments can offer you clearer skin and fewer flares and can liberate you from itching and flaking.
Taking a functional medicine approach that addresses your facial eczema contributors and triggers may help. Functional medicine investigates and treats root causes rather than taking an approach that only masks symptoms.
In this article, we’ll explore what potentially causes eczema, common triggers for face eczema, functional medicine approaches to treating the condition, and more.
Understanding facial eczema
To unpack the nitty-gritty of facial eczema, we have to dig into what eczema is in the first place and how facial eczema differs from eczema elsewhere.
What is eczema?
Eczema is really an umbrella term for a group of inflammatory skin conditions that cause skin irritation, such as itching, burning, flaking, oozing, and red, purple, gray, or brown patches, depending on your skin tone.
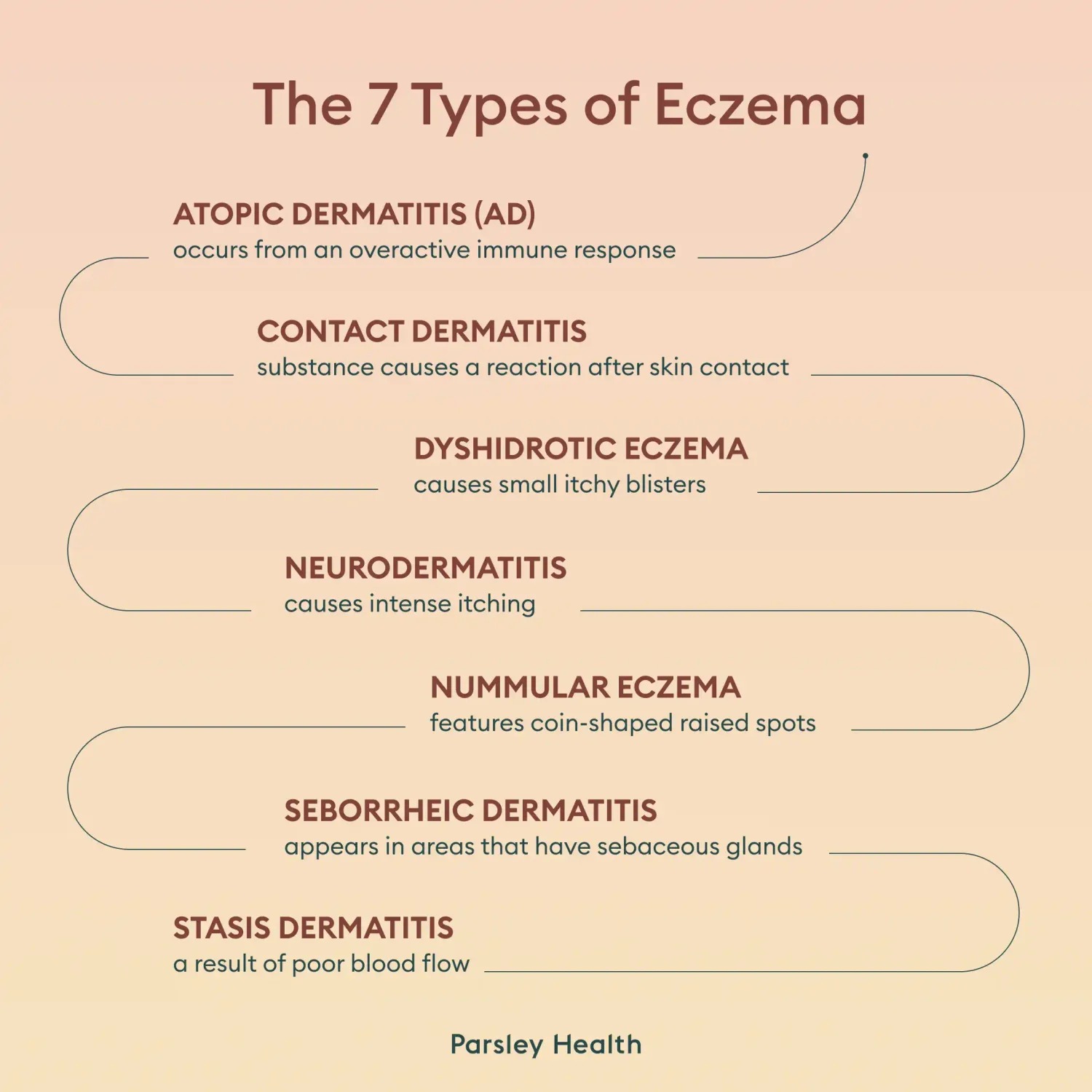
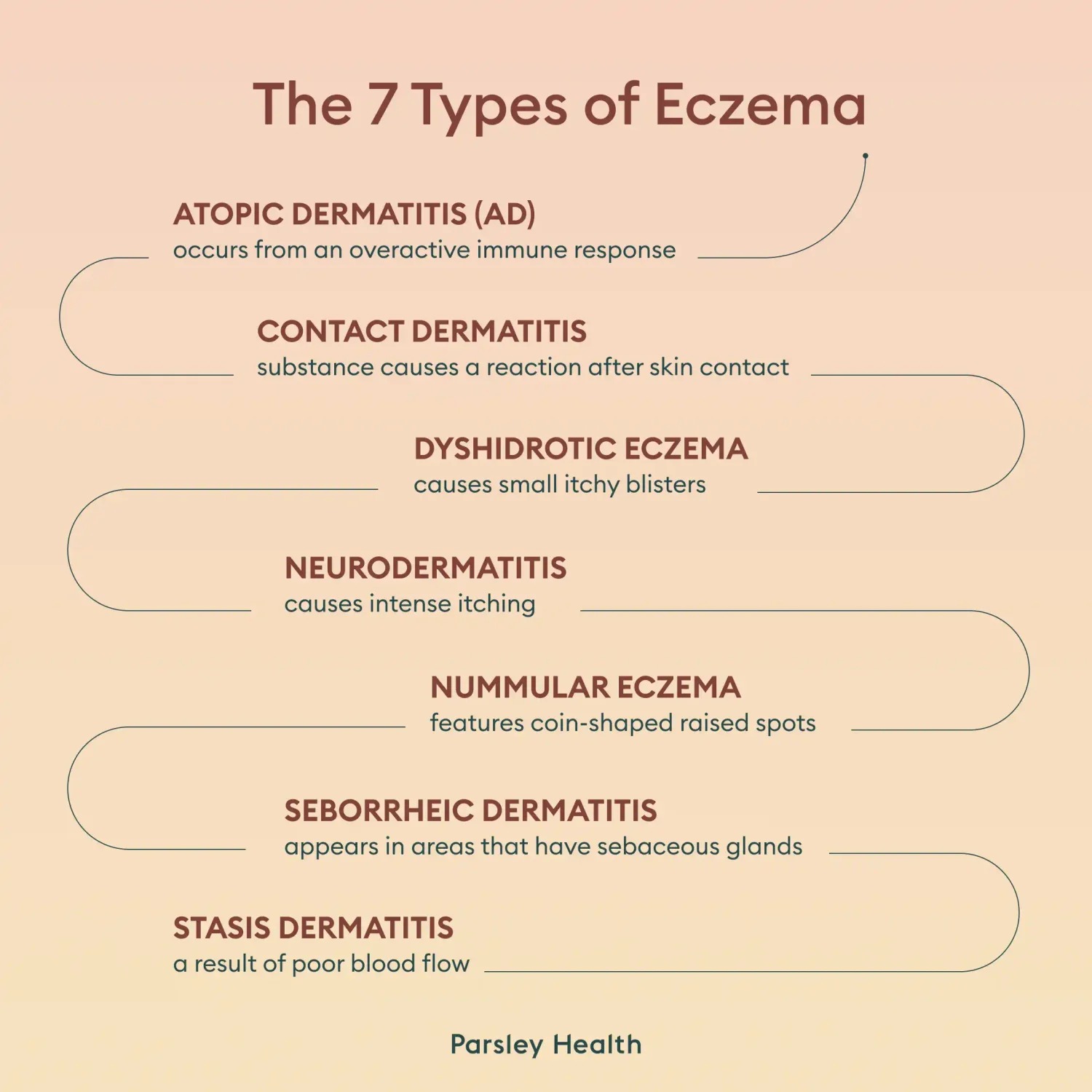
7 types of eczema
- Atopic dermatitis (AD) occurs from an overactive immune response that drives inflammation that damages the skin barrier.
- Contact dermatitis occurs when a substance causes irritation or an allergic reaction during or after skin contact.
- Dyshidrotic eczema causes small itchy blisters, usually on the hands and feet.
- Neurodermatitis causes intense itching. It usually appears in just a few thick patches on the body, and it may affect the eyelids. Excessive scratching can cause lesions that damage nerves.
- Nummular eczema features itchy and inflamed coin-shaped raised spots.
- Seborrheic dermatitis appears in areas that have sebaceous glands (glands that produce sebum, aka oil), including the face, scalp, and neck. A common trigger for this type is an overgrowth of a yeast that lives on the skin.
- Stasis dermatitis is generally a result of venous insufficiency (poor blood flow) in the lower extremities, leading to water and blood cells pooling in the lower legs, causing them to swell and become discolored.
How is facial eczema different from eczema elsewhere?
You can have any of the seven types of eczema, or multiple types that overlap, and some types of eczema may affect your face.
Facial eczema is the same as eczema that appears elsewhere, but it shows up on your cheeks, around the mouth, around the eyes, and in the nasolabial folds, and more. And it can present challenges.
- Visibility: Our faces are our most visible parts, so when eczema strikes, it can affect self-confidence and mental health.
- Texture and sensitivity: Facial skin tends to be more delicate and sensitive than skin on most other parts of your body, which can worsen irritation and make treatment more complex.
- Skin microbiome: The facial skin microbiome differs from the body’s skin microbiome, and it may be more prone to eczema exacerbations.
- Environmental exposure: Because of increased environmental exposure (e.g., pollution and ultraviolet radiation) and other factors, facial skin can lose more moisture, which could compromise the skin barrier, leading to eczema flares.
- Products: We tend to use more products on facial skin (e.g., cosmetics and skincare items), which could irritate already inflamed skin.
- Co-occurring conditions: Other skin conditions—such as acne and rosacea, melasma, actinic keratosis, vitiligo, psoriasis—also commonly affect facial skin, and these conditions may require different treatments from those of eczema and may cause additional irritation.
Common causes and triggers of facial eczema
“The biggest challenges I see with patients with facial eczema is not understanding what is causing their type of eczema and trying to treat it without direction,” says Dina Strachan, MD, a dermatologist.
The exact cause of eczema is unknown, and each eczema type likely has different or overlapping causes, according to the National Eczema Foundation.
Researchers believe genetics play a role in the development of eczema, since certain gene variants share links with the various types of the condition. Additionally environmental factors may play a role. Based on animal and laboratory studies, researchers have found that certain chemicals can induce eczema.
One prevailing theory on what drives eczema is that some people may be more susceptible based on genetics and that environmental and other factors then trigger eczema development and exacerbations.The following are some common triggers.
Genetic factors and atopic predisposition
Most research looking at genetic factors that may contribute to eczema focuses on atopic dermatitis. In a 2020 review investigating 73 research articles, scientists flagged 62 genes as having associations with atopic dermatitis. Additionally, children of parents who have allergic diseases are more at risk for eczema.
Skin barrier dysfunction
The stratum corneum (aka the skin barrier) is your outermost layer of skin, and it serves two key functions: keeping harmful substances out and sealing moisture in.
But in people with eczema, the skin barrier can be “leaky.” The gene variant Filaggrin (FLG) has associations with the development of atopic dermatitis, among other skin conditions. This gene codes for the filaggrin protein, which helps bind keratin filaments to strengthen skin cells.
When you don’t have enough filaggrin because of mutations in the FLG gene, then your skin barrier can develop gaps, leading to moisture loss.
Lipids (essential fats) are an important component of your skin barrier. But people with eczema may have less ceramide, a substance that helps trap moisture in the skin, leading to additional dryness.
Dryness can cause itching, which can tempt you to scratch, further degrading the skin barrier, creating a vicious cycle.
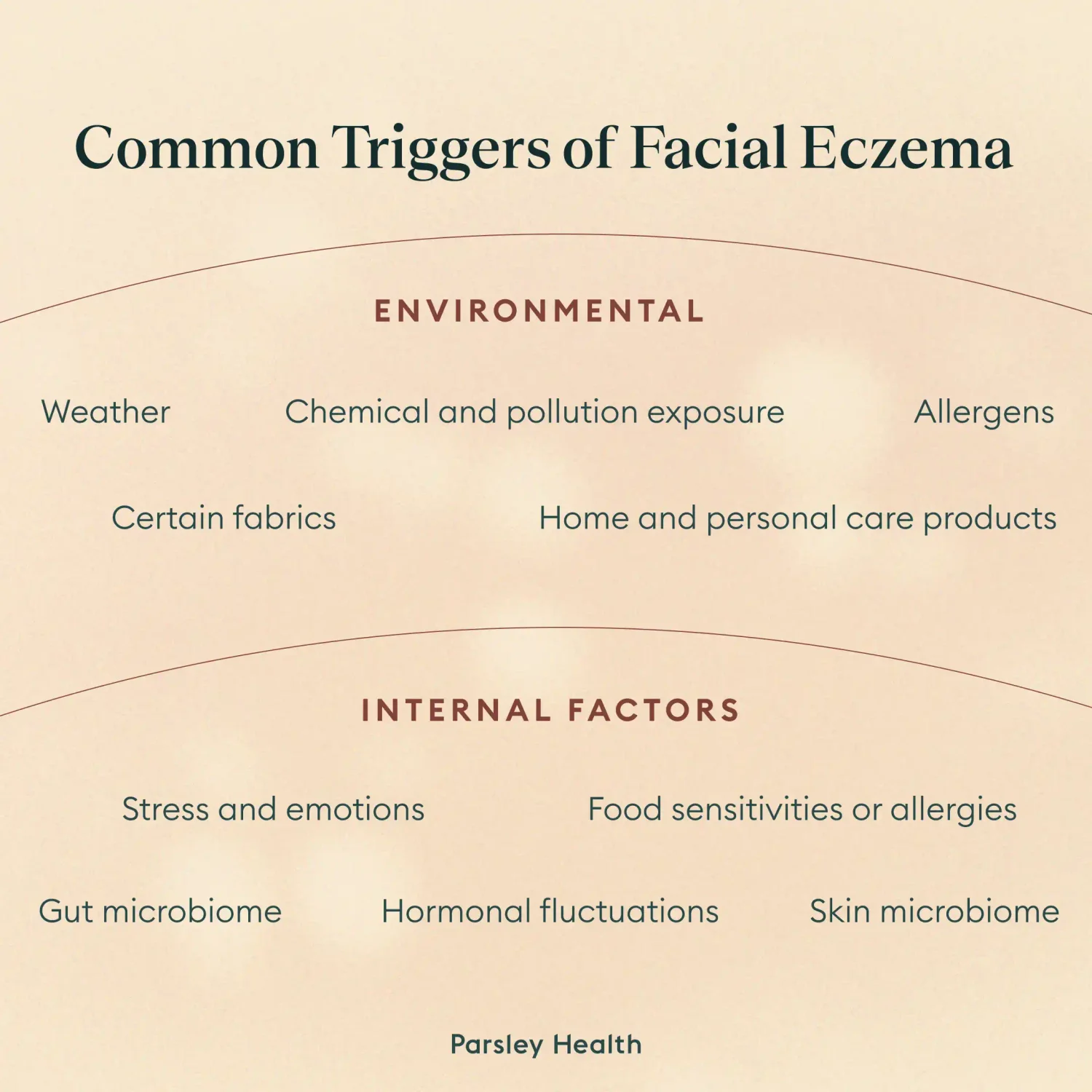
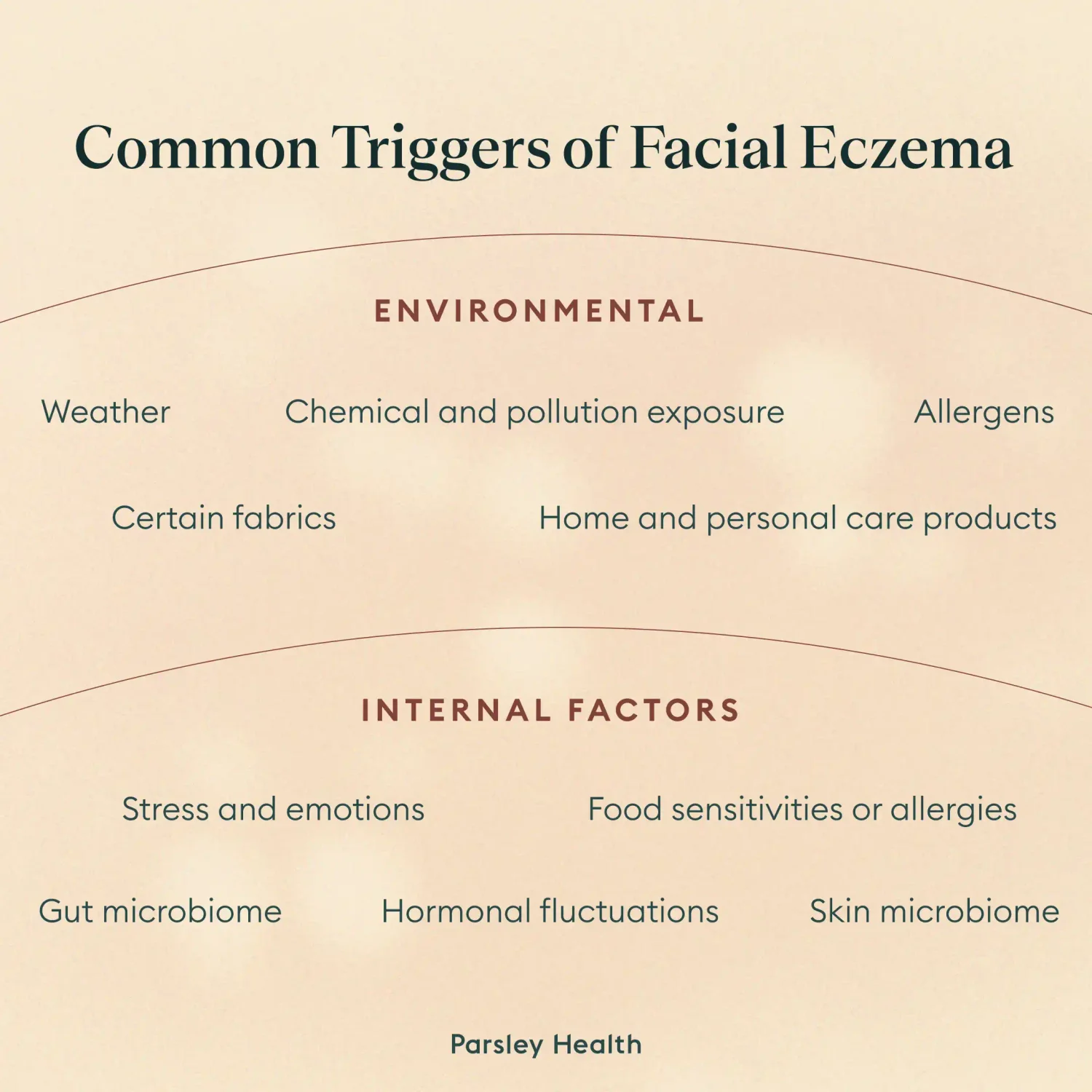
Environmental triggers
Several environmental factors may play a role in eczema development or triggers, including chemical and pollution exposure, climate or weather, personal care and household products, and allergens. Facial skin tends to be the most exposed to these concerns.
Chemical and pollution exposure
The National Institute of Allergy and Infectious Diseases has linked eczema to exposure to certain chemicals.
Through animal studies, researchers have determined that exposure to widely used chemicals called diisocyanates induces atopic dermatitis in mice. These chemicals are used in polyurethane products, including coatings, sealants, adhesives, and rubbery materials.
Large human studies looking at people’s history of eczema and pollution exposure (based on region) have found links between eczema and exposure to soot, sulfur dioxide, nitrogen dioxide, carbon monoxide, and fine particulate matter ( PM2.5).
Climate or weather
Though not a cause of eczema, your overall climate or a temporary weather pattern may also trigger a flare. For example, cold and dry air commonly cause eczema exacerbations. And sun exposure that irritates the skin may also irritate eczema patches. Additionally, climate issues, such as fumes from wildfires can trigger flares.
Irritants
Home and personal care products can also trigger eczema, especially contact dermatitis, by causing irritation or disrupting the skin barrier. Common culprits may include laundry detergents, household cleaners, shower or bath products, other topical skincare products, and more. Read on for how to find products that are eczema friendly.
Certain fabrics, such as wool or polyester, can also be irritating to eczema-prone skin. So be mindful of scarves and other facial coverings that could cause a flare. Likewise, other materials, such as metal, especially nickel from jewelry, tends to be an irritation culprit.
Allergens
If you have environmental allergies, such as to pollen, mold, dust mites, animal dander, or topical ingredients, exposure to these allergens may trigger eczema flares.
Internal factors
Just as external environmental factors can cause flares, so can factors going on inside your body, including food sensitivities, skin microbiome imbalances, gut microbiome imbalances, hormonal fluctuations, and stress.
Food sensitivities or allergies
Nuts, eggs, dairy, wheat, and soy are common eczema triggers for people with these specific food allergies. Additionally, food sensitivities or intolerances, such as to gluten, may play a role in eczema flares. However, dermatitis herpetiformis, which is linked to celiac disease, is a different skin condition that can mimic eczema.
If you have food sensitivities or allergies, your gut could play a role. A functional medicine practitioner can guide you on ways to support gut health, resolve “leaky gut,” and more. Tactics may include balancing the gut microbiome or undergoing a temporary elimination diet before slowly reintroducing foods one at a time to see if they cause your symptoms. The goal of any elimination diet is not to restrict foods but to help uncover any underlying causes contributing to your symptoms.
Skin microbiome
You have a whole community of bacteria, viruses, and fungi living on your skin. This community makes up your skin microbiome. Researchers have determined that the composition of the skin microbiome is different in people with eczema when compared to people without. Experts are still working on determining if these differences are contributors to eczema and how to address them.
Gut microbiome
Your digestive tract also has a unique microbiome, and it may affect your skin via the gut-skin axis, where the gut and skin communicate with each other.
In people with atopic dermatitis, some of the “bad” microbes that populate the gut are increased, while some of the “good” microbes are decreased. Therefore, a gut microbiome imbalance, often called dysbiosis, could be an eczema trigger.
Hormonal fluctuations
Hormonal changes, especially those associated with the menstrual cycle, perimenopause or menopause, pregnancy, and more, can trigger flares.
However, if you typically experience an eczema flare during the luteal phase, just before you get your period, you may actually have another condition called autoimmune progesterone dermatitis, which mimics eczema but is an autoimmune reaction to progesterone. This can also occur from progesterone taken as a hormone replacement therapy.
Stress and emotions
Stress or anxiety are not underlying causes of eczema, but they can be triggers. Some research shows connections between stress and impaired skin barrier function, likely because of increases in stress hormones, including cortisol. Stress may also affect the immune system, leading to an allergic response. And some research also shows that the stress response may be impaired in people with eczema.
How facial eczema is diagnosed
Clinicians diagnose facial eczema based on your symptoms, skin appearance, your suspected triggers, and other factors.A knowledgeable provider can take a thorough medical history, evaluate your skin if needed, and distinguish eczema from other skin conditions, such as rosacea. Then they can also offer treatment recommendations individualized to your needs and preferences.
Integrative treatment approaches
The right treatment for your facial eczema will be different from that of other people with the condition based on factors unique to you. Integrative treatment approaches may include avoiding triggers, adding topicals to help the skin barrier, taking supplements, and making lifestyle changes to diet and stress. Here are a few considerations.
Avoiding triggers
Avoiding all facial eczema triggers is tricky, especially since you can’t maintain control over all environmental factors, but you can with some.
The National Eczema Foundation features an index of products that have received the foundation’s Seal of Acceptance. Products with the seal have met rigorous standards as assessed by a board of eczema experts and have undergone testing for sensitivity, irritation, and toxicity. The searchable index can be a helpful tool for finding everyday products for your home or body that are less likely to trigger a flare.
Wearing sunscreen is a good idea for everyone, but it’s especially important if sun exposure worsens your eczema. And if you have environmental allergies, make sure they’re well-controlled. As for pollution, you can minimize your exposure by staying indoors on days when PM2.5 is high. Check an air quality app to monitor the levels in your area.
Skincare and topical care
Improving skin barrier integrity and function can also help with facial eczema. You can do this by moisturizing and preventing moisture loss with certain products. Skincare ingredients that can help include ceramides and vitamin B3, which is often called niacinamide on packaging.
Also avoiding super-hot or long showers and baths, in favor of more moderate water temps and shorter durations, can help prevent moisture loss. And engaging in a “soaking and smearing” routine can help. This means “smearing” your topical moisturizing products onto damp skin after bathing.
In some cases, however, you may need a prescription topical treatment to calm excessive inflammation or treat an infection.
Diet and gut health
If you have known food allergies or intolerances, steer clear of those items during snacks and meals. Other dietary changes may also be helpful, including eating anti-inflammatory foods.Since gut health and skin health are connected, addressing any gut microbiome imbalances under the guidance of a clinician can help.
Stress management and lifestyle adjustments
Stress and anxiety can exacerbate eczema, so stress management techniques, such as yoga, meditation, breathwork, and more, can be tools in your arsenal against flares.
Supplements and herbs
Some supplements can also boost gut and overall health and help stop eczema in its itchy tracks. A few that have shown promise in research include Zemaphyte (a Chinese medicine mixture of 10 herbs), kefir (a fermented milk drink) and freeze-dried whey with Cuscuta campestris Yuncker extract ( a combination of milk protein and a plant extract), though more research is needed.
Always talk to your health care provider before starting a supplement to ensure that it’s safe for you based on your underlying conditions, current medications, and other factors.
FAQ
How can I get rid of eczema on my face?
Eczema does not have a cure. However, if you are experiencing eczema, whether on your face or elsewhere, treatments can help alleviate symptoms and provide clearer skin. Holistic treatments include topicals to support the skin barrier, dietary changes, and supplements to reduce inflammation and support gut health. Avoiding triggers as much as possible is also crucial to prevent eczema flares. In some cases, you may need oral or prescription medications to prevent or treat flares.
What cream is good for eczema on face?
If you have facial eczema, you may wish to try creams that support your skin barrier function. Helpful ingredients include ceramides and vitamin B3, aka niacinamide.
What is the 3-minute rule for eczema?
The “3-minute rule” for eczema serves as a guideline for applying skin-barrier treatments as soon as possible (within three minutes) after bathing. After a moderate-temperature shower or bath, gently pat your skin with a soft towel but leave it damp. Then apply your moisturizer and other topicals. This routine helps hydrate the skin and lock in moisture, supporting your skin barrier.
What foods trigger eczema?
Some food triggers for eczema include common food allergies and sensitivities, such as to nuts, soy, dairy, eggs, and wheat. However, food allergies and sensitivities could also indicate underlying gut health issues that may need to be addressed.
Is eczema bacterial or fungal?
Eczema is not a bacterial or fungal infection. Instead, it is an umbrella term for a list of inflammatory skin conditions that cause itching and irritation, among other symptoms. However, people with eczema can develop skin infections from scratching that introduces harmful microbes or from having a compromised skin barrier and coming into contact with problematic bacteria or fungi. Also, an overgrowth of certain microbes on the skin can trigger an eczema flare.