Stress, believe it or not, can actually be a good thing. A healthy amount of cortisol, a primary stress hormone, can get you out of bed the day of a big presentation at work or help you metabolize your food. But when cortisol levels rise beyond a healthy threshold, your health—and life—can be negatively impacted. This is where a “cortisol detox” can come into play to help you naturally manage your cortisol levels.
A recent poll suggests 53% of Americans experience chronic stress, meaning over half of us are going through life with unhealthy cortisol levels. And if you’re experiencing high cortisol, the advice to stress less is probably more frustrating than helpful. What is useful is undertaking a cortisol detox. Ahead, discover what a cortisol detox is and natural ways to manage stress.
 Understanding Cortisol and Stress
Understanding Cortisol and Stress
Before we explain what a cortisol detox is, let’s bust a popular myth: cortisol and stress aren’t one in the same. Too much cortisol leads to what we label as stress, but that’s not its only purpose.
“Cortisol is a hormone produced by the adrenal glands that helps regulate the body’s stress response and energy levels, keeping you awake and alert throughout the day,” says Chester Wu, MD, a psychiatrist and sleep medicine expert with Rise Science.
In fact, this hormone plays a starring role in many systems in the body, including the:
- Nervous system
- Immune system
- Cardiovascular system
- Respiratory system
- Reproductive system
- Musculoskeletal system
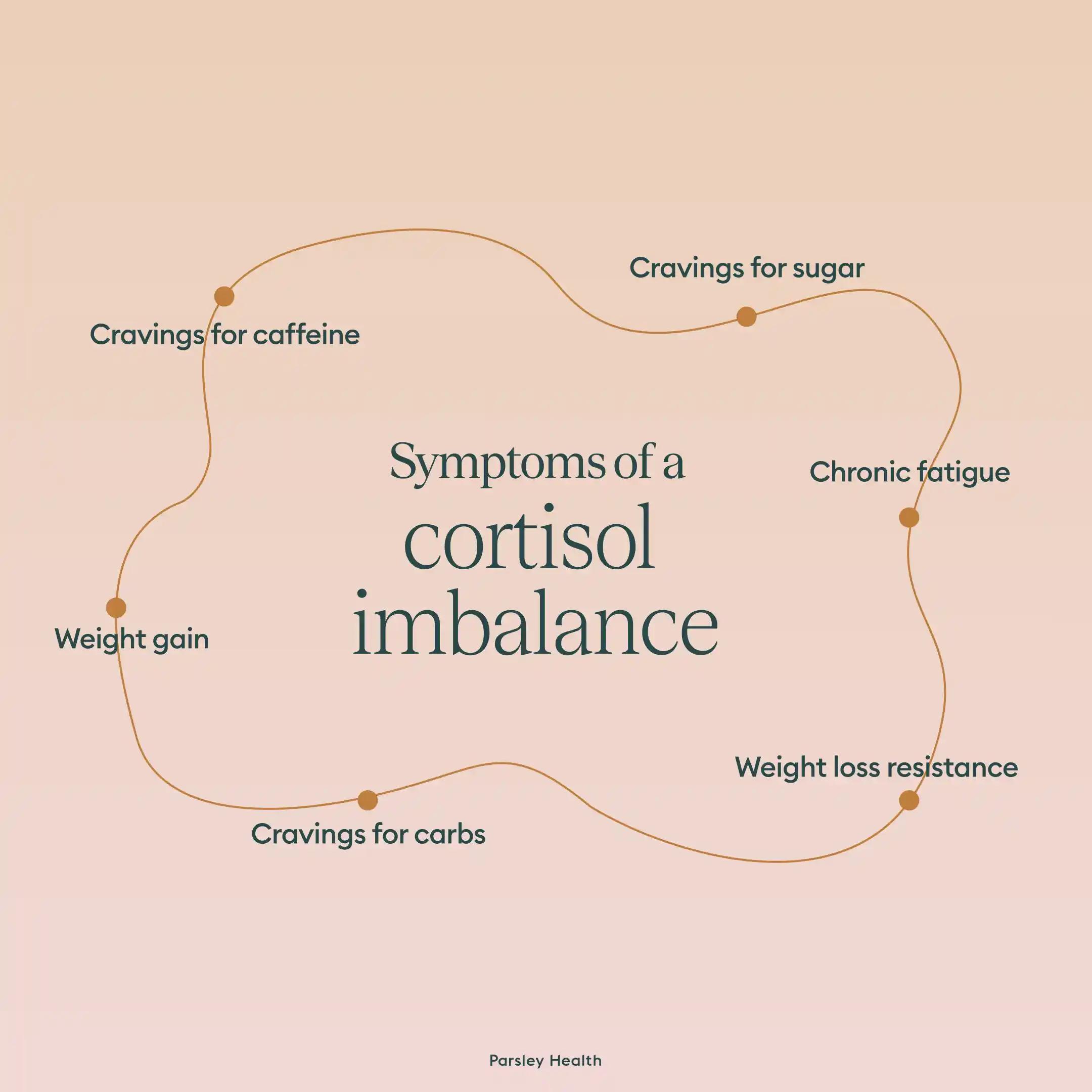
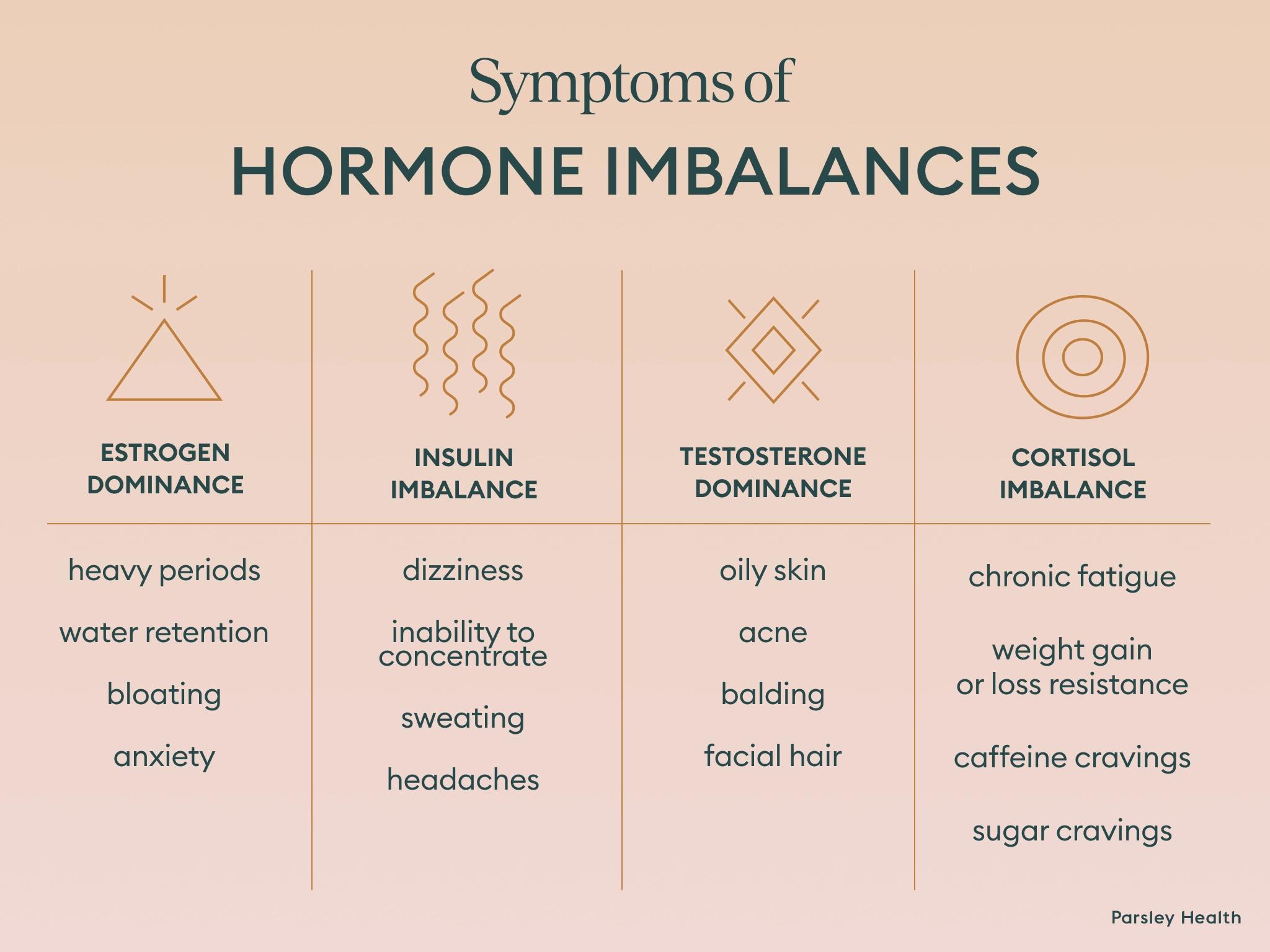
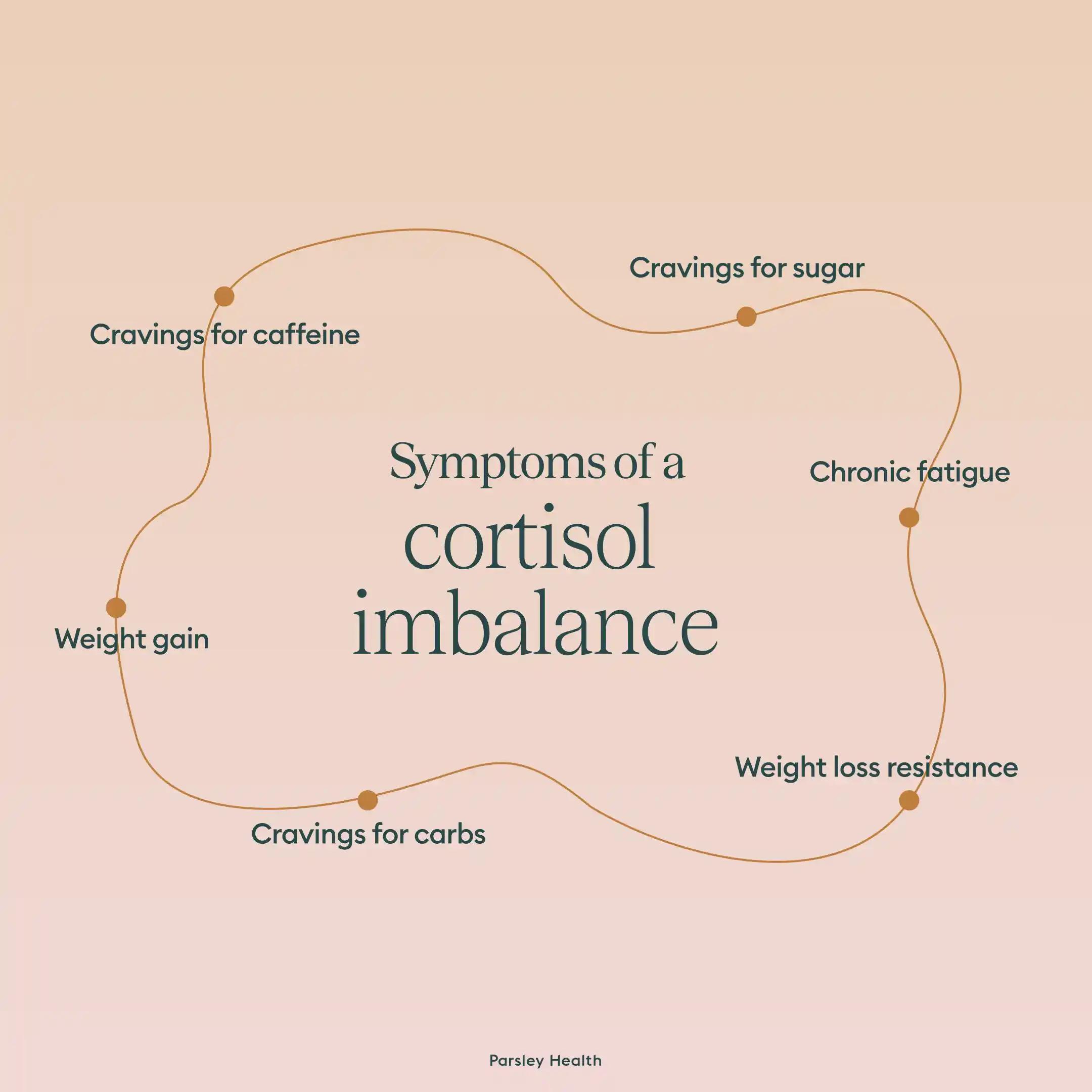
Whether cortisol plays the role of hero or villain for our health depends on if our cortisol rhythm is normal or chronically stimulated. Chronically stimulated cortisol has been linked to stress, anxiety, depression, diabetes, heart disease, and high blood pressure.
But before you panic (and unintentionally raise your cortisol levels), it’s important to note that like most hormones, cortisol is a natural part of being human. The key to a cortisol detox should NOT be to get rid of all stress, but to restore the normal cortisol rhythm.
 Dr. Wu explains, “While many think cortisol should be kept low at all times, it's actually important for cortisol to follow its natural rhythm—elevating in the morning to help you wake up and gradually decreasing throughout the day.”
Dr. Wu explains, “While many think cortisol should be kept low at all times, it's actually important for cortisol to follow its natural rhythm—elevating in the morning to help you wake up and gradually decreasing throughout the day.”
Chronic vs Acute Stress
When we initiate a cortisol detox, the aim should be to restore cortisol’s normal rhythm. A cortisol detox should focus on reducing chronic stress and developing a toolkit to deal with acute stress. What’s the difference between acute and chronic stress? Glad you asked.
Acute stress occurs when an external stressor causes a stress spike that disappears quickly. If you get stuck in a traffic jam while running late to work, that would be an example of acute stress.
Chronic stress is when those fight-or-flight feelings overstay their visit. Often, this is due to an ongoing external stressor, such as being laid off or marital problems. Untreated chronic stress is more likely to lead to more serious complications, like anxiety and depression, a weakened immune system, metabolic imbalance, and even a higher risk of mortality.
What Is A Cortisol Detox?
While it’s clear that chronic stress is less than ideal, a base level of cortisol is necessary for immune function, regulating metabolism, and other bodily functions. As a result, a cortisol detox should focus on getting cortisol back to its normal rhythm, rather than a state of overstimulation.
To do so, a cortisol detox is designed with a three-pronged approach:
- Implementing a diet that helps restore a normal cortisol rhythm
- Changing your lifestyle to reduce chronic stress
- Developing a toolbox of relief techniques to hone stress resilience whenever acute stress pops up
Below, we’ll dive into evidence-based practice for each prong. As you read, you can jot down notes on which ones may work well for your lifestyle and health. It may be helpful to create a list of different habits, foods, and stress relief techniques that you can pull from on a daily basis and/or when a stressor appears.
Nutrition and Supplements for Cortisol Detox
A healthy diet is the foundation for manageable stress levels. Francis Shih, MD, the medical director for Neuro Wellness Spa, recommends eating a balanced diet that’s heavy on whole foods and plant-based options and skimps on processed sugar.
However, the advice to “eat a balanced diet” is vague and not the easiest to follow. Luckily, researchers have pinpointed specific foods that can help lower cortisol.
Fiber
Fiber, a type of carbohydrate that keeps us full for longer, should be on our plates. It’s commonly found in legumes, vegetables, fruits, nuts, seeds, and whole grains. A stir fry of veggies, lentils, and brown rice, for example, would be a meal high in fiber. This wonder carb offers a variety of health benefits: improved gut health, lower risk of type 2 diabetes and heart disease, and enhanced mental health.
And, yes, that last benefit does encompass cortisol levels. The reason fiber impacts stress can be tricky to define, but multiple studies link fiber to lower levels of stress and anxiety.
Omega-3
Omega-3 is a fatty acid that provides the good kind of fat that our bodies use for a variety of functions. One of those functions? Regulating stress responses. In fact, participants in a 2021 study who took an omega-3 supplement had 19-33% less cortisol after four months than the study’s placebo group.
Along with supplements, Omega-3 is found naturally in:
- Most types of fish and seafood
- Flaxseed
- Chia seeds
- Walnuts
- Plant oils
- Eggs
- Yogurt
- Milk
- Soy beverages
Green Tea
By now, most of us are aware that too much caffeine increases cortisol levels. But replacing your morning cuppa joe or your afternoon cold brew is much easier when you have a healthier alternative. Enter green tea.
Green tea is associated with lower cortisol levels, and some research suggests drinking up to six cups of green tea a day may help manage stress. This is the only the case, of course, if the majority or all of those green teas are decaf.
Vegetables and Fruit
A diet high in fruits and vegetables has been associated with lower stress levels. Most likely, fruits and veggies are higher in certain minerals, vitamins, and flavonoids that naturally lower cortisol, though researchers are still exploring the “why” behind this relationship.
While most fruits and vegetables will work, researchers in Australia found some fruits and veggies were more likely to lower cortisol levels:
- Apples
- Pears
- Oranges
- Banana
- Cruciferous vegetables (i.e. broccoli and cauliflower)
- Legume vegetables (i.e. lentils and chickpeas)
B Vitamin Supplement
One reason fruits and veggies are beneficial for our mental health is their high concentration of vitamins. Going straight to the source (aka supplements) can be a good way to lower cortisol levels. But if you’ve ever scrolled the supplement aisle of a health food store, you know the options to choose from can be overwhelming.
While multiple vitamins and supplements have been linked to reduced stress, B vitamins are the best supported option—more specifically, vitamins B1, B6, B9, and B12. Some foods are also high in B vitamins, including, but not limited to, peas, nuts, chicken, bananas, oats, and milk.
Lifestyle Changes to Manage Stress & Naturally Improve Cortisol Level
If experiencing chronic stress, changing your lifestyle may help you feel more relaxed in your day-to-day life. While it’s not always possible to eliminate all stressors, such as a toxic job or a chronic illness in the family, there are habits you can implement to feel more in control of your emotions and stress levels.
Exercise
“Any physical activity that makes you break a sweat is a good way to destress,” says Dr. Shih. While any physical activity lowers stress, low intensity and medium/high intensity exercise impacts cortisol levels differently.
If looking to reduce cortisol immediately, low impact exercises, like Pilates and yoga, are your best bet. These workouts allow you to improve fitness and flexibility and to reduce stress during the workout.
High or moderate intensity exercises, such as running and high intensity interval training (HIIT), actually increase cortisol during and immediately after the workout, but that doesn’t mean they don’t have their place in a cortisol detox. If someone consistently engages in these exercise types, cortisol levels fall below the baseline “normal.” So going for a jog or trying out CrossFit may raise cortisol in the short-term but overtime, it builds stress resilience and lowers our normal stress levels.
Getting enough sleep
We’ve all woken up on the wrong side of the bed, something that can leave us cranky and full of worry and tension. Dr. Wu mentions that not getting enough sleep (or a good quality of sleep) elevates cortisol levels.
As a result, he recommends prioritizing sleep duration and quality. For length, the U.S. Office of Disease Prevention and Health Promotion, recommends adults sleep seven hours a night at minimum.
Sleep quality is defined as how satisfied you are with your “experience” sleeping. If you wake up multiple times during the night and feel groggy in the morning, for example, your sleep quality may be lower than if you wake up well-rested from an uninterrupted slumber.
Effective ways to improve sleep quality include:
- Stick to a specific bedtime and wake-up time
- Keep the bedroom cool and quiet
- Shut off electronic devices at least thirty minutes before sleeping
- Exercise regularly
- Avoid caffeine in the late afternoon or evening
Nature
Even five minutes in nature lowers stress and makes you happier. When you incorporate nature into your daily routine, whether that looks like an evening walk or eating breakfast in the backyard, it becomes a powerful part of your cortisol detox. If you live somewhere without a lot of green space, you may be able to get the same benefits by bringing nature to you; a 2021 study suggests any greenery, including houseplants, can reduce stress.
Get organized
A symptom of chronic stress is disorganization. Ironically, being disorganized can also stress us out even more. To stop this toxic cycle, clean up your physical space and stay on top of deadlines and digital information may help. Implementing effective organization techniques may be especially useful if your chronic stress is related to your work.
Growing old
The last tip isn’t a habit per se, but it is a lifestyle change that leads to less stress: aging. Typically, we see aging as an enemy to great health, but in the case of stress, we naturally become more resilient to external stressors as we age.
Again, there’s nothing you can do to implement this lifestyle change, but it’s comforting to know that the high cortisol levels you may be feeling now will decrease with time.
Natural Stress Relief Techniques
Changing habits is a great way to lower chronic stress. But when you’re in a stressful meeting at work, those eight hours of sleep or consistent workouts may not seem as helpful. In instances of acute stress, it can be helpful to have some natural stress relief techniques on hand.
Relaxation techniques
Sometimes, we need to press the reset button on our cortisol levels. Relaxation techniques that calm the mind and body are often the best way to do so. Typically, these techniques focus on bringing awareness back to the present moment and releasing any physical or emotional tension. They also stimulate nerves that help us relax, such as the vagus nerve.
Three common techniques include:
- Breathwork: taking slow, deep breaths allows you to stay in the present moment, calming the body and mind.
- Progressive muscle relaxation: with this technique, you tense and then relax different parts of the body, typically progressing from head to toe.
- Meditation: redirecting your thoughts via guided meditation or focusing on nothing is a great way to lower cortisol levels.
Laughing
Laughter is often the best medicine when it comes to stress. When we laugh, the body relaxes, and the bioactivities of cortisol are suppressed. In turn, this leads to a sudden decrease in active cortisol.
Next time you experience a stressful week or receive bad news, consider turning on your favorite sitcom or watching funny dog videos on Youtube—and don’t be afraid to laugh out loud.
Family and social support
A good conversation with a friend or family member can leave us feeling lighter, and there’s actual evidence to support the idea that feeling socially connected reduces cortisol levels. When we feel connected to others, we also have a support system to deal with life’s challenges.
Do something that makes you happy
An underrated way to reduce cortisol is to engage in a hobby or activity that makes you happy, according to Dr. Shih. Hobbies we enjoy lower the perceived stress in our lives and provide outlets to better cope with stressful situations.
Those exact hobbies will differ from person to person. So long as they don’t include unhealthy coping mechanisms (like alcohol or gambling), hobbies are a great way to manage stress. Consider this your permission slip to spend time crocheting, reading, or baking this week.
Take a walk (outside)
We’re already established that movement and nature reduce chronic stress, but it’s also effective when acute stress pops up. For maximum impact, use exercise and nature in tandem by walking in a nearby park or around the neighborhood.
To fully relieve stress, an hour-long walk in a forest or other nature (i.e. not urban or suburban setting) may be best, though any amount of walking outdoors can lower cortisol levels.
Creating a Personalized Cortisol Detox Plan
A successful cortisol detox plan will pull from all three prongs (diet, lifestyle changes, and stress relief techniques). But that doesn't mean you need to implement every idea in the article right now—or ever.
Individual responses to stress vary, meaning your cortisol detox plan should be customized to how you respond to stress and what you enjoy. If, for example, high levels of cortisol make you feel the flight part of the fight or flight response, running may be a great hobby. Conversely, someone else may find stress relief via regular yoga classes.
For maximum effectiveness, a cortisol detox should be planned in collaboration with a doctor and with your lifestyle and health in mind. The right doctor will be able to discern your personal symptoms and determine the best path forward, given those symptoms, your lifestyle, and any underlying medical conditions.
Frequently Asked Questions (FAQs) About Cortisol Detoxes
How do you flush cortisol out of your body?
To “flush out” cortisol (or more accurately lower cortisol), you should focus on cultivating a lifestyle and diet that supports a normal cortisol rhythm and decreases stress. This often consists of prioritizing sleep, daily movement, and meals high in whole foods and low in processed sugar.
What lowers cortisol immediately?
One of the most effective ways to lower cortisol immediately is to practice a relaxation technique that directs your attention inward by focusing on your body rather than the stressor at hand. Meditation and breathwork are two of the most effective techniques. If you’re having difficulty focusing during meditation or breathwork, laughter also works well.
How to get rid of cortisol belly?
Cortisol’s rhythm impacts many parts of our body, including gut health. If you have extra weight around the belly due to stress, focus on eating more whole foods and partaking in fewer ultraprocessed ones. When paired with stress relief techniques, such as daily exercise or meditation, this diet can be effective.
What is a cortisol detox diet?
A cortisol detox diet is one that’s high in whole foods, low in processed foods. Specific whole foods to prioritize include sources of fiber, omega-3 fatty acids, and vitamin B. Eating a high concentration of fruits and veggies may also help restore or maintain cortisol’s normal rhythm.
Final Thoughts
Cortisol isn’t the enemy. It’s a useful hormone that helps regulate our metabolism, lets us know when we’re in danger, and supports healthy immune system functioning. But chronic stress leads to cortisol stimulation, an unwanted guest that can wreak havoc on our mental and physical health. A cortisol detox can give that guest the boot.
When building your own cortisol detox, consider diet and lifestyle changes to reduce chronic stress and build a toolkit of stress relief techniques when an acute stressor pops up. A doctor who understands how to naturally relieve stress can help you select the right changes and relief techniques for your specific lifestyle and medical conditions. At Parsley Health, our doctors are adept at this and can help you restore cortisol’s normal rhythm. Learn more about how Parsley Health can support your cortisol detox and restore your hormonal balance.
 Understanding Cortisol and Stress
Understanding Cortisol and Stress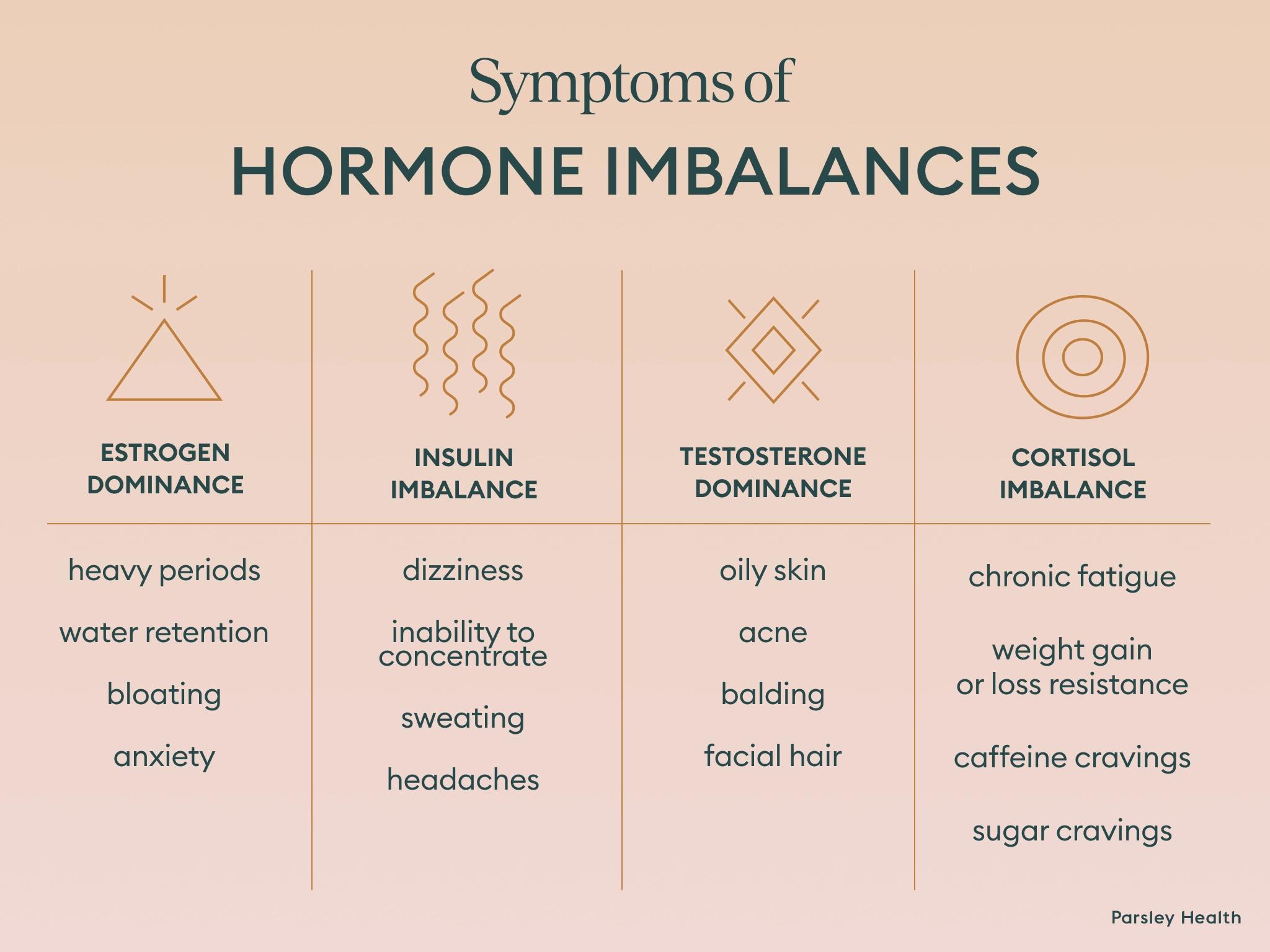 Dr. Wu explains, “While many think cortisol should be kept low at all times, it's actually important for cortisol to follow its natural rhythm—elevating in the morning to help you wake up and gradually decreasing throughout the day.”
Dr. Wu explains, “While many think cortisol should be kept low at all times, it's actually important for cortisol to follow its natural rhythm—elevating in the morning to help you wake up and gradually decreasing throughout the day.”






