A functional medicine doctor uncovers and addresses the root cause of a symptom or disease and treats the whole patient, rather than focusing on just one organ or bodily system. They also help patients prevent disease processes and optimize their overall health and well-being.
When I was 21, my OB-GYN diagnosed me with endometriosis, a systemic inflammatory condition that’s now dubbed as one of the 20 most painful conditions a person can have. Endometriosis has no cure, and although treatments can help with management, they are often inadequate, so I’ve spent the last 25 years managing my endo with a mix of conventional and functional medicine. Both are valuable tools in my arsenal for maintaining optimal health and comfort while dealing with a chronic condition.
Conventional medicine has served me well in emergencies, multiple abdominal surgeries to preserve pelvic organ health, and more. Functional medicine has served me well by helping me to optimize my overall health, support my reproductive/sex hormones, and keep inflammation at bay to reduce endometriosis flare-ups.
My situation is just one example of how conventional medicine and functional medicine can complement each other. In this article, we’ll explore what functional medicine is, what functional medicine doctors do, how functional medicine aligns with conventional approaches, and when you might wish to see a functional medicine doctor.
What is functional medicine?
The Institute of Functional Medicine (IFM), founded in 1991 by Susan and Jeffrey Bland, PhD, gives this concise definition: “Functional medicine provides a framework to systematically identify and address the underlying processes and dysfunctions that are causing imbalance and disease in each individual. By understanding a patient’s genetic, environmental, and lifestyle influences, functional medicine clinicians create personalized interventions that restore balance, health, and well-being.”
We can look to the term “functional” to further explain what functional medicine is. “Every symptom arises from the imperfect discharge of function,” wrote Dr. Willoughby Wade in an 1871 article in the medical journal Lancet. More than a century and a half ago, Dr. Wade outlined some of the frameworks for what’s considered functional medicine today. Essentially, he pointed out that when a symptom arises in our bodies or brains, it originates from a source of dysfunction that, if not addressed, may later turn into a disease state. Functional medicine aims to understand the source of the dysfunction and restore function where possible to prevent disease.
The condition type 2 diabetes (and its many symptoms) offers a great example. Type 2 diabetes can be traced to mitochondrial dysfunction. Mitochondria are the powerhouses of our cells, and if they don’t work properly, lots of problems can arise, including high blood sugar and tissue and organ damage. Mitochondrial dysfunction occurs within the body long before someone is diagnosed with type 2 diabetes. A root-cause approach can help prevent the escalation of the disease.
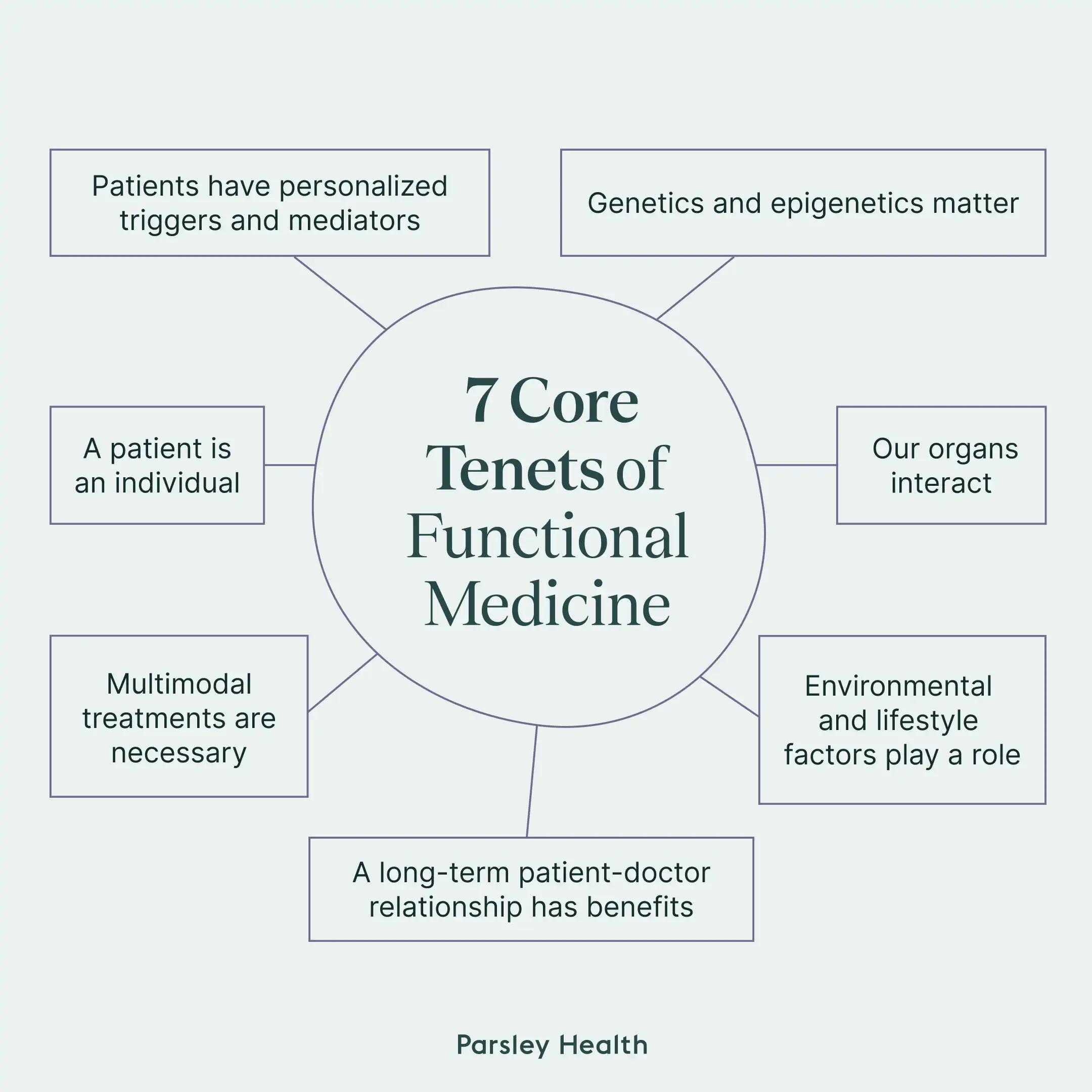
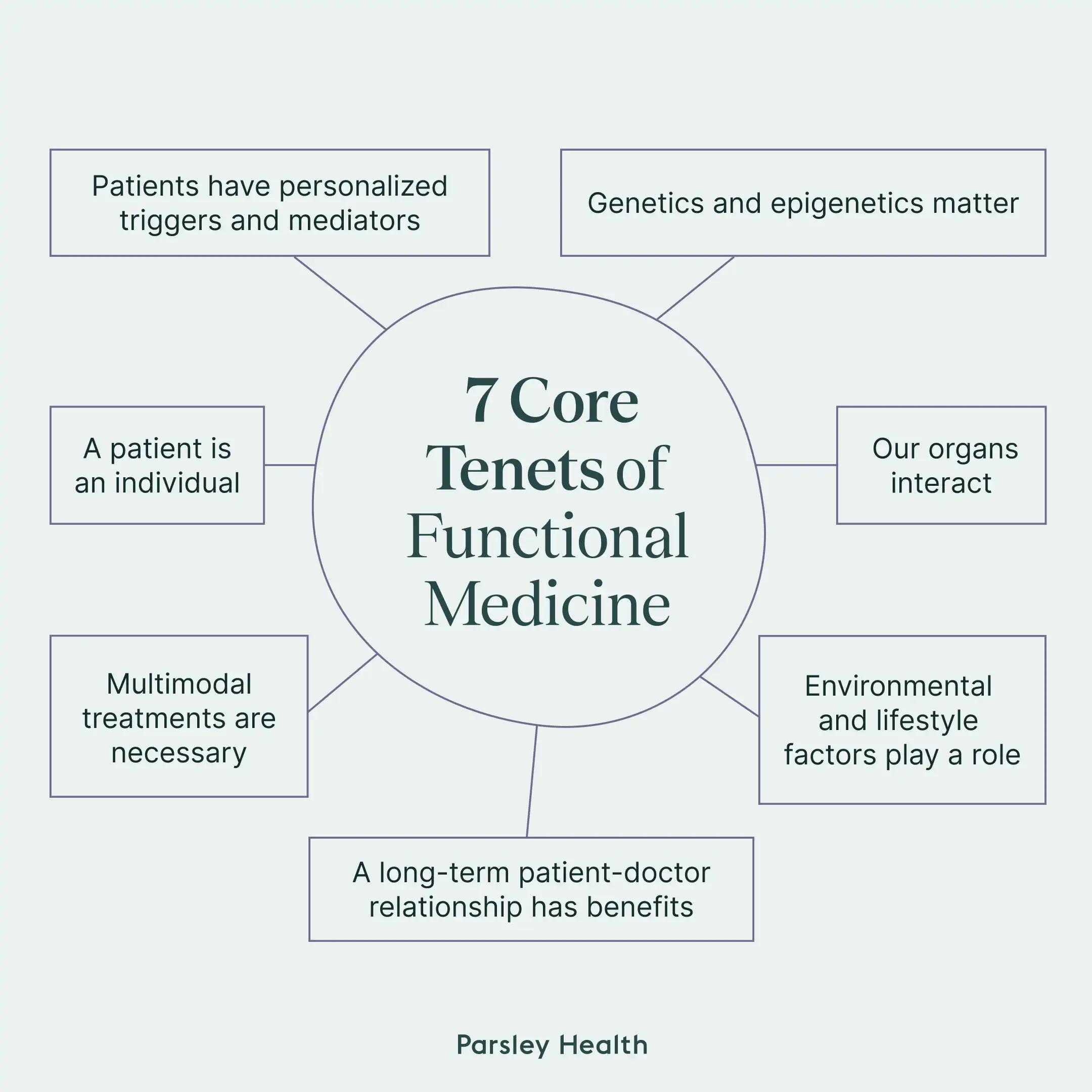
Functional medicine focuses on getting to the root cause to help manage or resolve symptoms, prevent condition progression or disease development, and more. Functional medicine follows seven core tenets or principles.
7 core tenets of functional medicine
1. Genetics and epigenetics matter.
Based on our genetics, we may have a higher risk for some conditions. Research suggests that genetics determine about 20 percent of our health, while the other 80 percent involves epigenetics, or how our environment and lifestyle factors alter our gene expression. Functional medicine helps you change environmental and lifestyle factors.
2. Our organs interact.
Conventional medicine often takes a bucketed or siloed approach. We can observe this by simply looking at all the “ologists” in a hospital or clinic system. You’ll find neurologists (for nervous system issues), cardiologists (for heart issues), dermatologists (for skin issues), and gastroenterologists (for digestive issues). These clinicians typically specialize in one organ or system (aka focusing on their “bucket”). However, that siloed approach ignores the fact that a condition often affects multiple organs and systems.
As an example, an endocrine issue such as polycystic ovary syndrome (PCOS) can also manifest as a skin issue with acne, unwanted hair growth, etc. Rather than simply treating the skin issue, a functional medicine approach addresses the endocrine dysfunction in multiple ways, which then helps address the skin symptoms.
3. Environmental and lifestyle factors play a role.
So many factors determine the state of our health, including our environmental exposures to things like pollution or toxins, our lifestyle factors including diet and exercise, and even our social structure including our support system. These factors all influence our gene expression in positive or negative ways. Functional medicine recognizes this and helps you modify factors to optimize your health.
4. Patients have personalized triggers and mediators.
Along with endometriosis, I also have chronic migraine. (Lucky me!) My migraine triggers and what brings me relief during an attack will be different from the next person’s. As someone who’s had these diagnoses for a long time, I also have a different relationship and experience with my health status than the next person has with theirs. Functional medicine recognizes these individual factors and takes a personalized approach to treatment, management, and more, while also taking into consideration cultural and other dynamics that intersect with health.
5. Multimodal treatments are necessary.
A condition or symptom may require several different treatments, rather than just one. For example, for migraine, I require prescription medications, supplements, diet and lifestyle interventions, and more. Migraine is a complex neurological condition that does not have a cure. However, many people do find they can reduce their triggers through lifestyle changes. For example, better blood sugar control may help reduce the frequency of attacks and reduce reliance on medications in some people. Through the help of lifestyle interventions, I’ve had periods in my life where, although I still have this chronic neurological condition, I’ve experienced a reduction in attacks. Functional medicine approaches a condition from as many angles as possible to find the right treatments for each person.
6. A patient is an individual.
As patients facing health concerns, we’re all unique, for many of the reasons already mentioned above. Functional medicine takes an “N-of-1” approach. (The “N” number in a clinical trial is the number of participants.) This means that instead of considering what works for most people with a specific symptom or condition based on research, functional medicine considers the research and takes a scientific approach to explore what will work for you and your unique circumstances.
7. A long-term relationship has benefits.
Functional medicine focuses on the patient-clinician relationship, where the clinician gets to know the patient and all their individualized health factors over time, works with them to develop a personalized treatment plan and changes the plan if something isn’t working or if a new step is necessary.
What is a functional medicine doctor?
As you may have guessed, on a basic level, a functional medicine doctor practices functional medicine. They may be one of the following:
- Doctor of Medicine (MD)
- Doctor of Osteopathic Medicine (DO)
- A naturopathic doctor (ND)
Functional medicine doctors are fully licensed doctors who have gone through traditional medical school and training. Other functional medicine practitioners may have nurse practitioner (NP) and physician assistant (PA) credentials or even a doctor of chiropractic (DC) .
How functional medicine aligns with conventional medicine
Functional medicine and conventional medicine aren’t in opposition to each other. In fact, they can complement each other quite well. My journey with migraine can serve as a good example. Migraine is a chronic neurological condition for which I see a conventional neurologist. I take several prescription medications, some to help prevent migraine attacks and some to help relieve a migraine that’s already in process. I also get BOTOX for migraine.
But I have also worked with functional medicine clinicians to help me better understand my triggers and prevent exposure to them and to help me revamp my diet to correct nutrient deficiencies associated with migraine, reduce inflammation, and improve my gut microbiome—since the bacteria and fungi that live in the gut appear to be altered in people with migraine. Functional medicine clinicians have also helped me to reduce stress, improve sleep, support hormonal balance, and even change my exercise routine, all to help with migraine. My conventional neurologist has asked me about some of these topics but has tended to focus mostly on the medication component for treatment.
Additionally, migraine and endometriosis have strong associations. My functional medicine doctors have always acknowledged this and explored the connections as part of my treatment plans. Conventional medicine doctors, in my personal experience, have rarely discussed the conditions together.
I don’t want to come across as if I’m dissing conventional medicine. I honestly don’t know where I’d be without it. But I feel the same way about functional medicine. I truly need both in my life to manage migraine and endometriosis. Managing chronic conditions is a full-time job for the patient. For me, the difference comes down to this: Functional medicine focuses on helping me control what I can to improve my quality of life.
Another way that conventional and functional medicine differ is that functional medicine often takes a preventive approach, whereas conventional medicine tends to treat disease states.
I used type 2 diabetes as an example mentioned above. So let’s explore that one a bit further. Doctors diagnose type 2 diabetes based on glucose tests. Before developing type 2 diabetes (fasting blood glucose that’s 126 mg/dL or higher) a person will have prediabetes (a fasting blood glucose of 100 mg/dL or higher). In conventional medicine in the United States, doctors consider your blood glucose to be normal if it’s below 100 mg/dL. However, if your fasting blood glucose is 98, you’re likely on a trajectory to develop prediabetes. This illustrates that a “normal” test result may not be “optimal.” However, in the United States, conventional medicine rarely treats prediabetes, let alone someone who almost has prediabetes.
Yet, if you have prediabetes or are close to developing it, you might have noticed symptoms associated with insulin resistance, such as weight gain, cravings or feeling hungry all the time, fatigue, and more. Since functional medicine takes a root-cause approach, a functional medicine doctor would evaluate your symptoms, incorporate testing where necessary, determine that you are on a trajectory toward prediabetes, and then help you implement lifestyle changes to lower your fasting glucose level to a more optimal number.
A functional medicine clinician may use several different tools and techniques to address the root cause of your symptoms, help you achieve optimal health, and more.
One common tool is the Functional Medicine Matrix, which involves nodes. Nodes are crucial aspects of human physiology and health. The matrix is a tool to help your clinician understand your medical history, lifestyle factors, triggers, and more, and to organize any imbalances according to the nodes of functional medicine. This visualization or mapping tool helps your clinician connect the dots between seemingly unrelated symptoms or issues and gain a better picture of your health and well-being.
Nodes of functional medicine
- Structural integrity. This node addresses cellular integrity, tissue structure, and the musculoskeletal system.
- Psychosocial (mental, emotional, spiritual). This node concerns your well-being, emotional regulation, and more.
- Assimilation. This node focuses on digestion, absorption of nutrients, and the health of the gastrointestinal microbiome.
- Defense and repair. This node focuses on your immune system, inflammatory processes, and your body’s ability to heal itself.
- Energy. This node concerns how well your body converts food to usable energy. It encompasses mitochondrial function (mitochondria are the powerhouses of your cells), ATP production (your body’s usable energy), and factors influencing fatigue and overall energy regulation.
- Communication. This node concerns how well your cells send and receive messages. This node involves chemical messengers like hormones and neurotransmitters.
- Transport. This node involves the cardiovascular and lymphatic systems, focusing on the circulation of nutrients, oxygen, and waste products throughout the body.
- Biotransformation and elimination. This node relates to detoxification processes, metabolic byproduct processing, and waste elimination through various bodily systems.
To help develop the matrix unique to you and understand what’s going on with your body, your provider may incorporate diagnostics, such as comprehensive blood panels, genetic testing, nutrient deficiency testing, hormone testing, microbiome testing, and more.
They will also spend time chatting with you to gain an understanding of when your symptoms started, any triggers, life events (such as traumas or stressors), and any other factors that may play a role in your health. They’ll also ask you about your lifestyle and fill in sections for sleep and relaxation, exercise and movement, nutrition and hydration, stress and resilience, and relationships and networks.
To collect even more information about you and get a complete picture, your clinician may also incorporate technology, such as continuous glucose monitors, sleep trackers, food logging apps, activity trackers, and more.
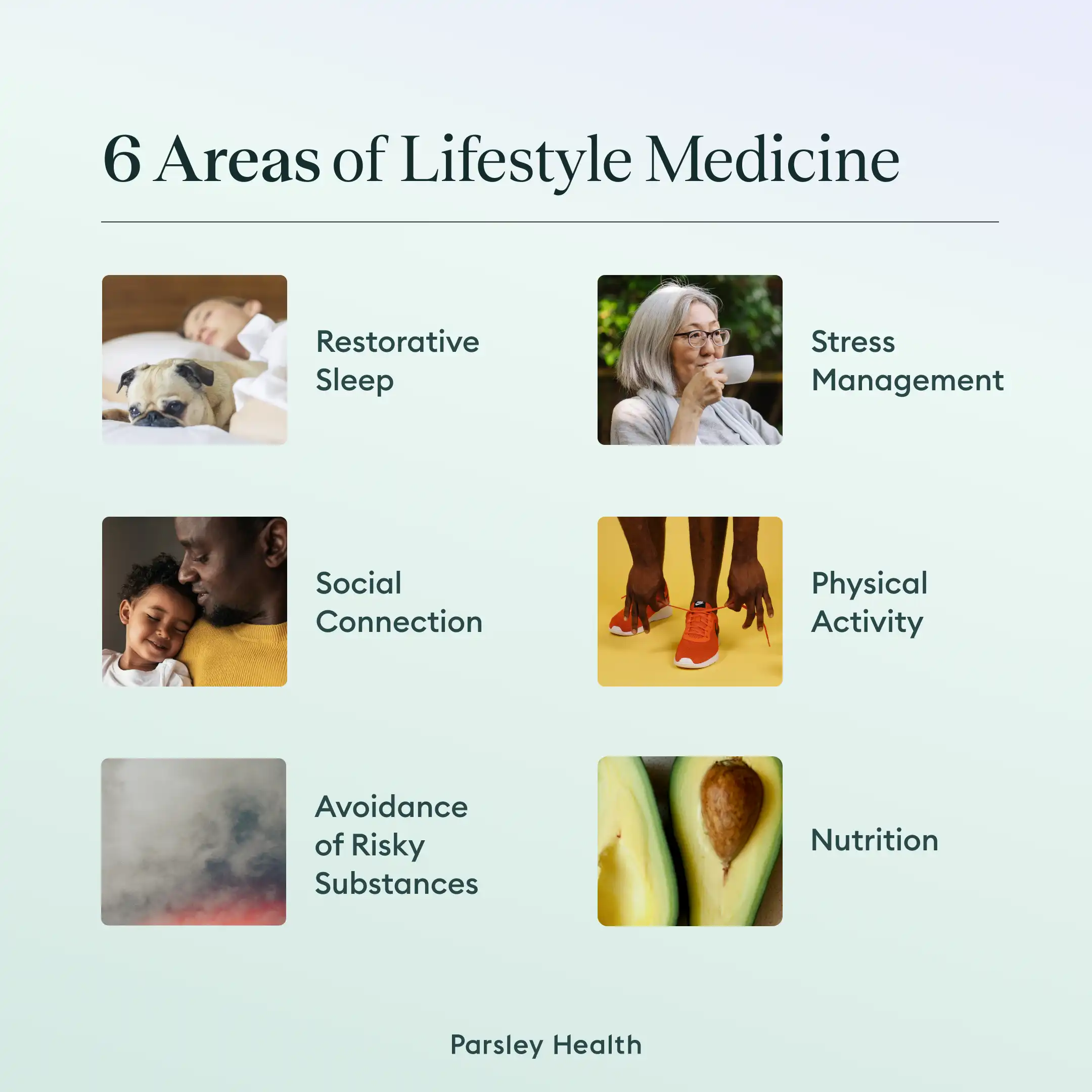
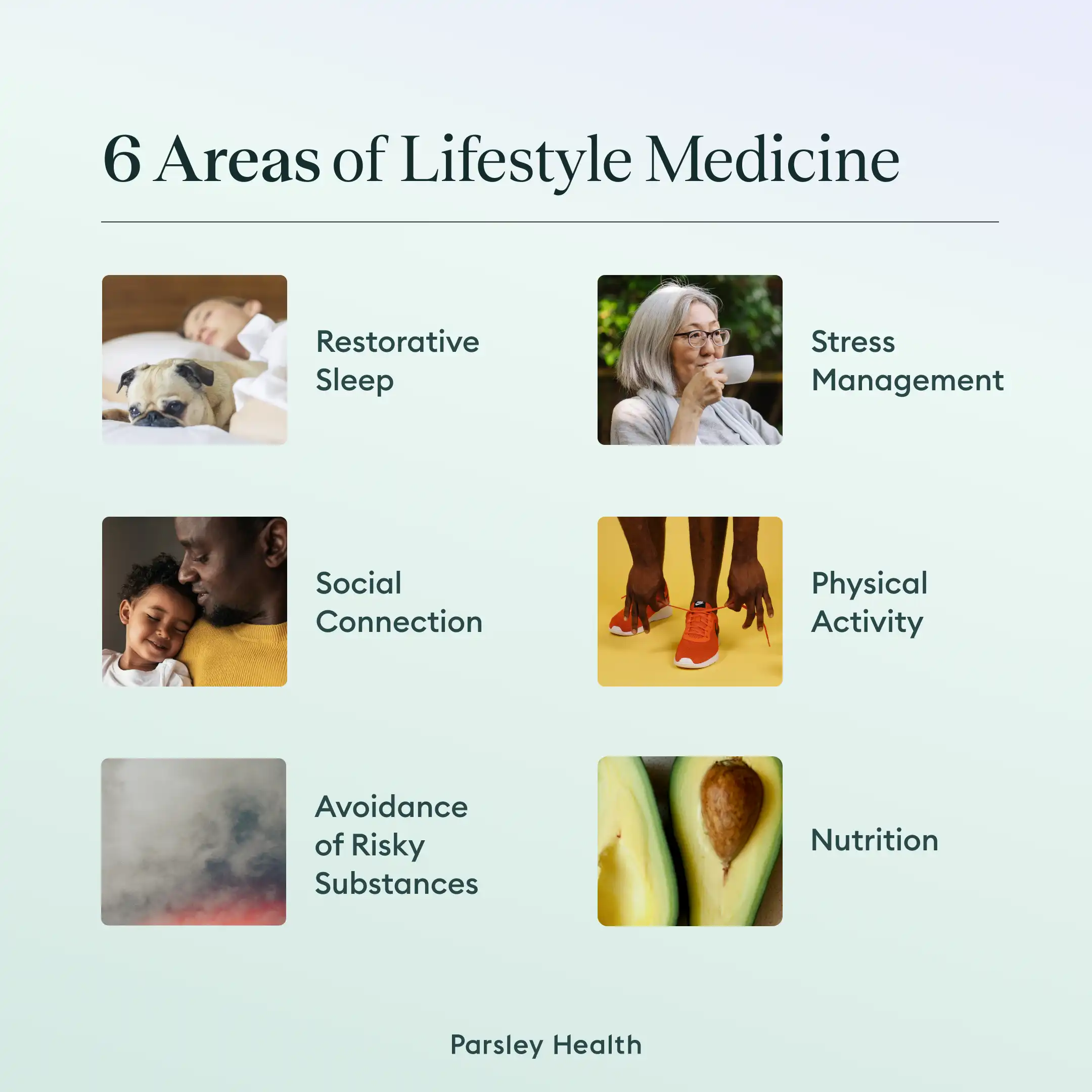
Your functional medicine clinician will then develop a treatment plan that’s unique to your needs for optimizing your health. They may include elements of what’s called “lifestyle medicine” to help. This involves focusing on lifestyle changes in six key areas to help prevent, reverse, and treat symptoms or diseases. Your functional medicine doc or their colleagues can even serve as a coach to help you dial in helpful lifestyle changes.
6 areas of lifestyle medicine
- Nutrition. This area focuses on the intake of nutrient-dense, minimally processed foods.
- Physical activity. This area focuses on getting adequate exercise.
- Stress management. This area focuses on reducing stress and boosting resilience to it.
- Restorative sleep. This area focuses on practicing good sleep hygiene habits and getting seven to nine hours of quality sleep per night.
- Social connection. This area focuses on the importance of having a support network and gleaning life purpose.
- Avoidance of risky substances. This area focuses on eliminating as much as possible exposure to pollution, toxins, and harmful substances, including tobacco and alcohol.
Criticisms and challenges of functional medicine
Functional medicine is not without its criticisms. One criticism is that it lacks standardization. The Institute of Functional Medicine, however, does have a certification program. The FMCP-M credential, for example, certifies those with MD, DO, ND, NP, and PA credentials.
Another criticism is that functional medicine isn’t based on scientific evidence. This is not true. Functional medicine practitioners use a systems biology approach, which looks at the larger picture by putting pieces together rather than examining pieces separately. In other words, functional medicine looks at the whole person rather than just an individual organ or system to see what might be going on.
And yet another criticism has to do with cost. Insurance companies don’t always cover functional medicine expenses. This means patients may have to pay out of pocket for services, sometimes with a membership fee. One argument against this criticism is that since functional medicine has a major preventive component, you may spend less on healthcare in the long run if you utilize this approach and prevent or reverse dysfunction before it becomes a disease state. Likewise, functional medicine also treats disease by getting to the root cause, meaning you may be able to correct some elements of dysfunction of existing disease and reduce your overall healthcare costs.
When to see a functional medicine doctor
Many people see a functional medicine doctor when a symptom or disease arises and they want to get to the root cause and address the underlying issues. By the time I saw my first functional medicine doctor, I already had my endometriosis diagnosis. I knew that I couldn’t cure the disease, but I could take steps to help alleviate my symptoms and optimize my overall health and well-being, which would ultimately improve my quality of life.
You can see a functional medicine doctor even if you are completely healthy or symptom-free. A functional medicine clinician can help you continue to optimize your health or uncover any “lurking” issues (such as a vitamin deficiency or low level that could cause issues down the road). They can also help you understand your risk factors for certain diseases and help you take a preventive approach.
Key Takeaways
- Functional medicine doctors take a root-cause approach to health, by addressing any underlying dysfunction that may be causing a symptom or disease.
- Functional medicine doctors also help patients prevent disease by lowering their risk factors and optimizing their health and well-being.
- Functional medicine takes a different approach or uses a different philosophy than conventional medicine, but functional medicine doctors are conventionally trained doctors with medical education.
- Conventional medicine and functional medicine can complement each other.
- If you are interested in giving functional medicine a try, reach out for a free consultation with Parsley Health.
FAQ
What is the difference between a functional medicine doctor and a regular doctor?
The main difference between a functional medicine doctor and a “regular” or conventional doctor is their philosophy. Conventional medicine doctors treat symptoms and diseases. Functional medicine doctors help get to the root cause to resolve, reverse, or manage the issue. Functional medicine doctors also treat the whole patient, whereas conventional medicine doctors tend to focus on the affected organ or system.
What is the downside of functional medicine?
One potential downside of functional medicine is cost. This is because your health insurance company may not cover functional medicine appointments or treatments. (Parsley Health partners with health insurance providers, and you will always know the price of each test or intervention to avoid any surprises.) Some functional medicine providers may offer membership fees that help alleviate expenses. And since functional medicine aims to get at the root cause, you may save on healthcare in the long run.
Is functional medicine legitimate?
Yes, functional medicine is legitimate medicine. Functional medicine doctors are conventionally trained doctors who did get their degree in conventional medical school before they trained in Functional Medicine.
What is the purpose of a functional medicine doctor?
The purpose of a functional medicine doctor is to treat the whole patient (rather than just an individual organ or bodily system) and to address the root cause of a symptom or disease, rather than to simply treat the issue. In some cases, diseases can even be resolved. Prediabetes is one example. In other cases, as with migraine, you may still have the condition but enjoy more relief and improved quality of life.
What is functional medicine used for?
Functional medicine is used to get to the root cause of a symptom or disease. It’s also used for maintaining optimal health and preventing disease processes in the first place. In some cases, diseases can even be resolved. Prediabetes is one example. In other cases, as with migraine, you may still have the condition but enjoy more relief and improved quality of life.