This article contains additional reporting by Angela Myers.
Almost everyone who gives birth experiences postpartum hormone fluctuations and while it’s new, it’s normal. That said, you should know what’s happening in your body and why, so we talked to two Parsley Health experts about what to expect from your hormones after you give birth, how long these changes will last, and signs of hormone imbalance after pregnancy.
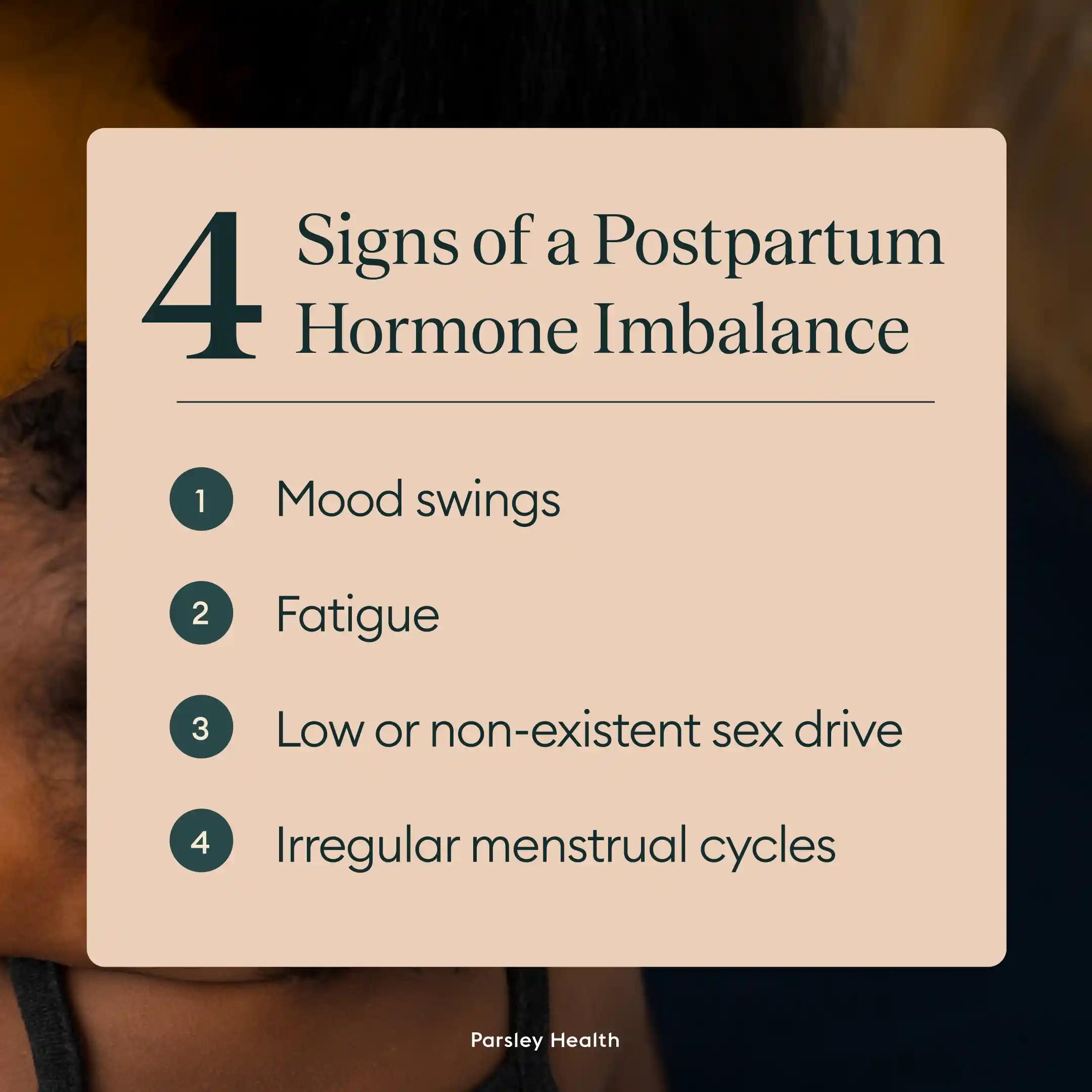
Signs of a Hormone Imbalance After Pregnancy
If you’ve recently given birth, your body is going through natural hormonal fluctuations that might make you feel a little different (on top of, you know, having a baby.).
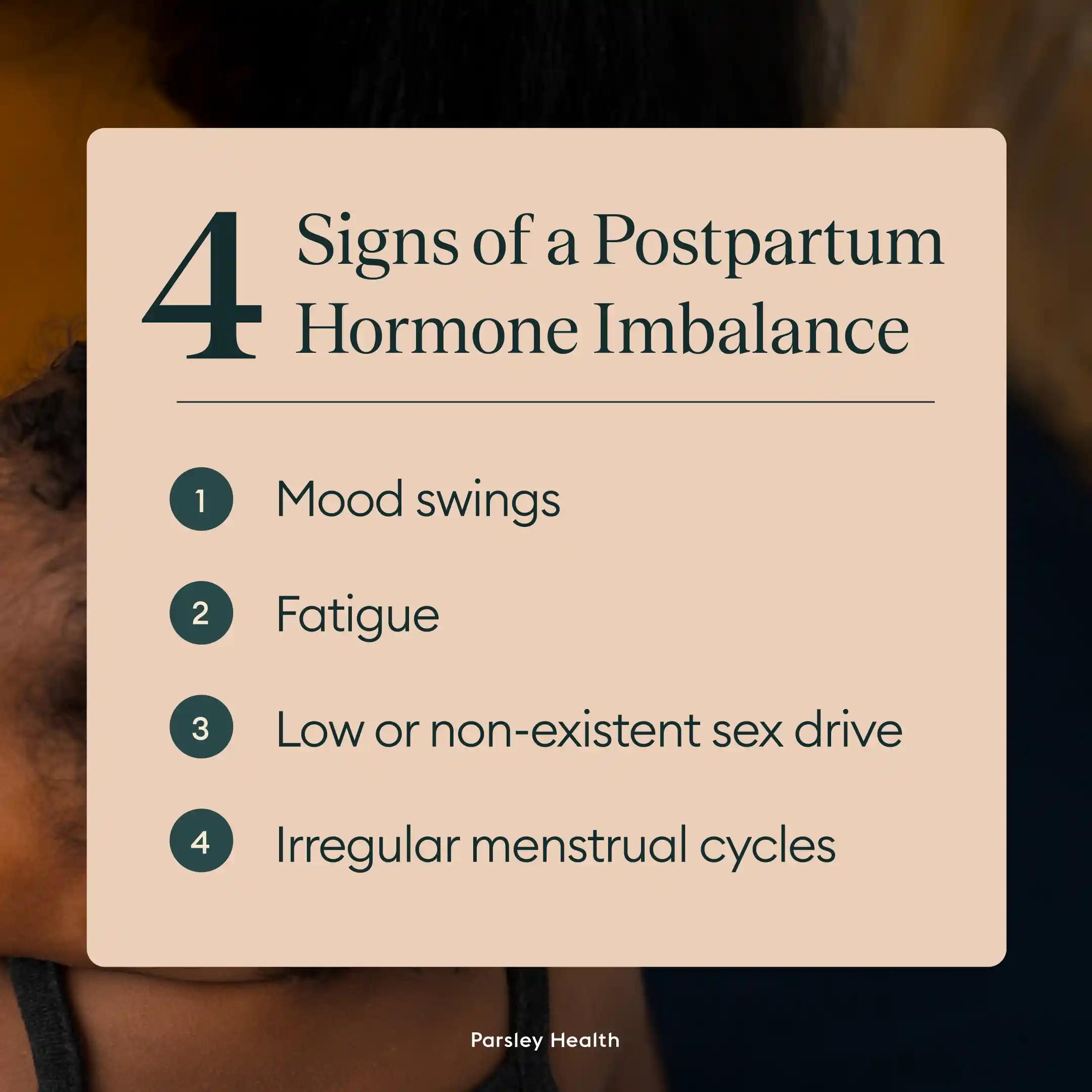
Postpartum hormonal imbalance symptoms can include:
- Mood swings
- Fatigue
- Low or non-existent sex drive
- Irregular menstrual cycles
Mood Swings
We've all heard of postpartum depression, a condition where a mother feels depressed after giving birth due to hormonal fluctuations. Postpartum depression is diagnosed in one in six new moms. Diagnosis or not, you can still experience mood swings, the baby blues, or anxiety after giving birth.
Fatigue
Exhaustion is a constant companion for parents, especially when postpartum. If feeling fatigued, sleep can do wonders, but for obvious reasons, it’s the most challenging to prioritize. Taking naps when you can and enlisting childcare support from friends, family members or childcare providers. These drug-free ways to get better sleep may also be helpful.
Low or Non-existent Sex Drive
Breastfeeding hormones can lower a new mother's sex drive and may even cause vaginal dryness and pain during sex. Usually, hormones and your sex drive return to normal once you're done breastfeeding.
Irregular Menstrual Cycles
Having an irregular period is normal after giving birth. For many new mothers, it can take months to get back to a normal flow, and even longer if you continue to breastfeed past the six month mark.
Weight Gain
Gaining weight while pregnant is normal. Usually, half that weight disappears six weeks after childbirth and the rest comes off over the next few months.
Christina Kang, a former health coach at Parsley Health encourages patients to avoid worrying about weight loss for the first 3 to 6 months after giving birth. “With patience, good nutrition, and moderate exercise, much of the weight will come off on its own over a period of time. When people are overly restrictive, the body may hold on to excess weight in order to have enough fuel to continue making breast milk,” she says.
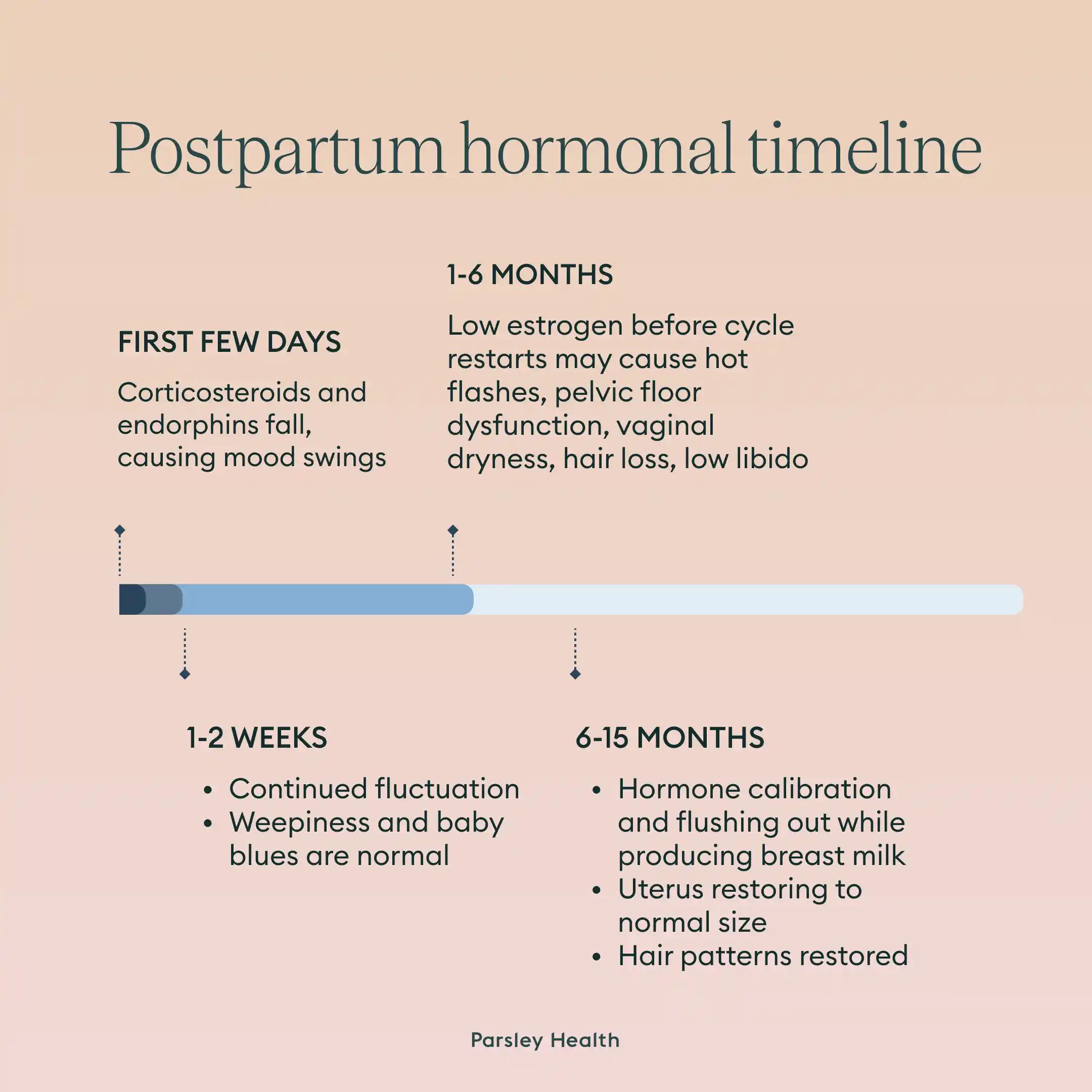
Timeline of Postpartum Hormonal Changes
According to former Parsley clinician Elizabeth Milbank, MD, MPH, several different hormones are responsible for the physical and emotional changes that women experience during delivery and postpartum.
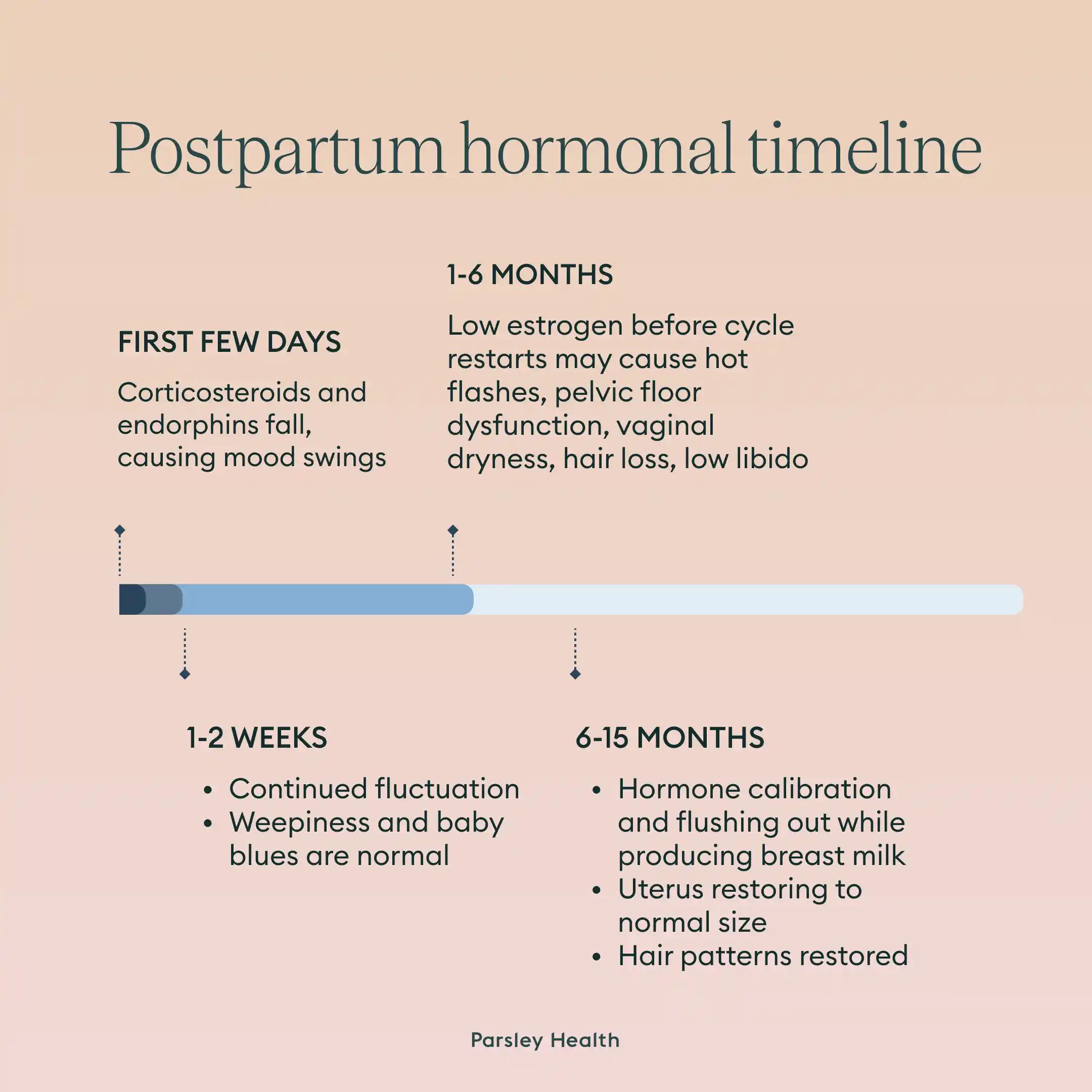
Immediately After Birth
Endorphins rise during labor, reach a peak immediately after delivery, and decline postpartum. High endorphin levels help women cope with the process of birth and may help women feel more alert, attentive and even euphoric after birth, but as they fall in the first few days postpartum, they too may contribute to mood swings, says Dr. Milbank.
Corticosteroids also reach a peak during labor and decrease significantly within three hours postpartum, making this an emotionally vulnerable period.
1 to 2 Weeks After Delivery
Within a few weeks of giving birth, many women experience the so-called “baby-blues”—where women can feel weepy, tearful and overwhelmed, says Kang. The moving and shifting of these hormones can be distressing, but it’s normal to experience them in the first few weeks after delivery.
1 to 6 Months After Delivery
Low estrogen levels—which stay low until a woman starts cycling again, and may last throughout the duration of breastfeeding—can contribute to postpartum hot flashes, pelvic floor dysfunction, vaginal dryness and low libido. Hair loss, or telogen effluvium, is another common symptom that can happen between one to six months after delivery.
In addition, the ongoing production of relaxin during breastfeeding—the hormone produced during pregnancy to soften the joints and ligaments in order to make space for the growing baby—may contribute to joint laxity.
6 Months to a Year After Delivery
“This hormone calibration can go on for many months with the production of breast milk, the uterus slowly moving back to normal size, and the body flushing itself of excess hormones,” Kang says.
Normal hair patterns are also typically restored 6 to 15 months after delivery, adds Dr. Milbank.
When to Seek Help
Any woman experiencing postpartum imbalances should lean on doctors and health coaches to ensure they're taking care of their mental and physical health. In fact, postpartum care often begins before delivery.
“When taking care of patients during their pregnancy, I always do a session in the third trimester to discuss postpartum care, nutrition, movement, mental health and lactation support (if they plan to breastfeed) and I am in close touch with my patients postpartum to make sure they have access to the support they need,” says Dr. Milbank.
It's especially important to seek medical help if experiencing persistent depression or symptoms of thyroid disease (both hyper- and hypothyroidism). Ask for a full panel of thyroid tests, including antibodies. If you have a history of thyroid disease then it is especially prudent to get this full panel done.
Hypothyroidism can occur postpartum due in part to certain changes in the immune system, Kang explains.
Frequently Asked Questions
How long does it take for hormones to balance after giving birth?
While we often think of the six week postpartum mark as a time when women can go back to work, have sex, and exercise, the truth is postpartum hormone imbalance can last for much longer. Many women experience imbalances up to three months after they stop breastfeeding.
How to fix postpartum hormone imbalance?
Usually, hormones will return to pre-pregnancy levels on their own, especially if you’re taking care of yourself with a healthy diet, plenty of sleep, and managing stress.
That being said, if symptoms of postpartum hormone imbalance are severe or last three to six months after you stop breastfeeding, visit a healthcare provider to see if there's any complications and to create a treatment plan. That plan may include working with a therapist to address postpartum anxiety or depression or with a postpartum doula or baby nurse.
How do I know if I have a hormone imbalance after pregnancy?
After giving birth, it's normal for hormones to be imbalanced. The exact symptoms you experience due to this imbalance and how long they last depend on a variety of factors, including baseline health pre-pregnancy, delivery method, gut health, diet and lifestyle, stress levels, thyroid health, and genetics.
How to know if hormones are imbalanced?
If hormones are imbalanced, you'll most likely experience mental or physical symptoms. Common ones include low libido, anxiety, depression, cysts or fibroids, weight gain, and chronic fatigue.
When should I check my hormones after pregnancy?
Most likely, you won't need to check your hormones after pregnancy, though you should be aware they will fluctuate postpartum, leading to different physical and mental health needs. However, if the symptoms you experience become severe or persist three to six months after breastfeeding ends, reach out to your doctor who will be able to check your hormone levels and evaluate you for postpartum depression, postpartum anxiety, and other serious issues.
How long does the pregnancy hormone stay in your body after birth?
While symptomatic hormonal fluctuations making you feel imbalanced can last in your body for months after giving birth, the pregnancy hormone human chorionic gonadotropin (hCG) sticks around for less time. It typically disappears from your system seven to 60 days after giving birth.
Does breastfeeding cause hormonal imbalance?
Breastfeeding primarily impacts two hormones, prolactin and oxytocin. Both are important for producing breast milk, and oxytocin also produces a state of calm within the mother. Prolactin, however, can leave a new mom feeling fatigued.